Hello everyone,
I am writing on antibiotic resistance as a global threat in the public health sector.
"Welcome my son, what is the problem? I am not fine, said Tunde. I am having a swelling in my left ear, it's seriously painful and I'm having headache. Sorry my dear, it should be a boil, the mum replied. There is Ampicillin on the center table, use one capsule and relax, you will be alright, pẹ̀lẹ́. Tunde's pain persisted for 2 days and his dad suggested he should consult a doctor. He was diagnosed for Otitis (middle air inflammation) and was successfully treated with Ceftriaxome."
This indicated that the bacterium that caused the otitis is resistant to Ampicillin.

Antibiotic drugs Pixabay Image :CCO Licensed
According to Singh, (2014) emergence of resistance in bacteria and other pathogenic organisms is a natural phenomenon which could neither be predicted nor contained. However, the process can be influenced by actions and inactions of man such as irrational use of antibiotics by humans. In that case, we are responsible for the spread of antibiotic resistance. The genes that is responsible for resistance are found in the DNA of the organisms. These genes could be innate (inbuilt) or acquired from other organisms.
The Pre-antibiotic Era
Before the discovery of antibiotics, man (young and old) suffered from enormous bacterial infections which led to their death in and outside hospitals. There were little the medical officers could do as there were no medicines to treat the infections. Even though the immune system could fight against some bacteria, many were still strong enough to defeat people's immunity.
The American Academy of Paediatrics (2015) reported that before antibiotics, 90% of children with bacterial meningitis died. Among those children who lived, most had severe and lasting disabilities, from deafness to mental retardation. Streptococcal throat infection was at times a fatal disease, and ear infections sometimes spread from the ear to the brain, causing severe problems. Other serious infections, from tuberculosis to pneumonia to whooping cough, were caused by aggressive bacteria that reproduced with extraordinary speed and led to serious illness and sometimes death.
The Discovery of Antibiotics
The discovery of antibiotics was accidental but diligence and curiosity by the scientists led to the glory. Antibiotic (penicillin) was discovered in 1928 by Alexander Fleming (a British Bacteriologist) at St. Mary's Hospital, London. Fleming was investigating Staphylococcus aureus that cause boils, sore throats and abscesses. Before he left for a 2-week vacation, Fleming unintentionally left a plate (petri dish) with cultured S. aureus on the laboratory bench and never placed in the incubator as intended.

When he returned from holiday, he began to sort through the petri dishes. He noticed something unusual on one plate. It was dotted with colonies, save for one area where a certain mould was growing. The zone immediately around the mould (Penicillium notatum) was clear, as if the mould had secreted something that inhibited bacterial growth. Fleming reported his observations as an inhibition or prevention of bacterial growth in areas affected by the 'mould juice'. Although he could not isolate the active compound (mould juice) but name it as penicillin coined from Penicillium notatum.
After Alexander Fleming’s 1928 discovery of penicillin, Howard W. Florey and Ernst B. Chain researched further and the outcome of their research enabled the testing and production of the drug. The discovery of penicillin and other antibiotics was a major achievement of the 20th century in the field of medicine. Fleming’s legendary discovery of penicillin changed the course of medicine and earned him a Nobel Prize in 1945 together with Howard Florey and Ernst Chain.

Penicillium notatum Wikimedia Common : Author: Crulina 98 Under CC License 3.0
Antibiotics have successfully prevented or treated infections that can occur in patients who are receiving chemotherapy treatments; who have chronic diseases such as diabetes, end-stage renal disease, or rheumatoid arthritis; or who have had complex surgeries such as organ transplants, joint replacements, or cardiac surgery (Gould and Bal, 2013).
Emergence of Antibiotic Resistance
It might be surprising to you to learn that resistance to antibiotics was identified even before Fleming's drug hit the shelves. The first clinical application of penicillin came in the early 1940s, but the discovery of beta-lactamase (a bacterial enzyme capable of destroying penicillin) preceded that revolution by a few years. The microbes were always one step ahead. As early as 1960, it was clear that overuse of antibiotics was driving the emergence of resistant species (Swain, 2011).
During the World War II, penicillin was successfully used for treatment of some bacterial infections. Shortly thereafter, penicillin resistance became a substantial clinical problem, so that, by the 1950s, many of the advances of the prior decade were threatened. In response, new beta-lactam antibiotics were discovered, developed, and deployed which restored some confidence. However, the first case of methicillin-resistant Staphylococcus aureus (MRSA) was identified in the United Kingdom and in United States in 1962 and 1968 respectively (Ventola, 2015).
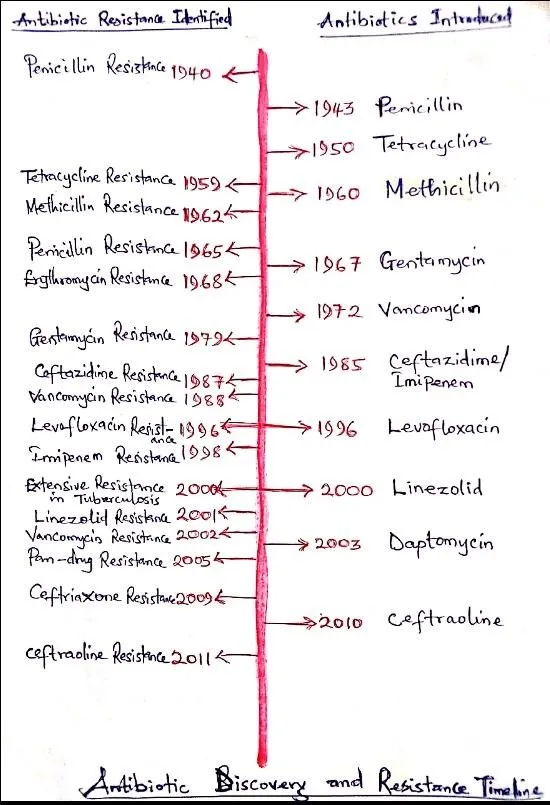
In 1972, vancomycin was introduced into clinical practice in 1972 for the treatment of methicillin resistance in both S. aureus and coagulase-negative staphylococci. It had been so difficult to induce vancomycin resistance that it was believed unlikely to occur in a clinical setting. However, cases of vancomycin resistance were reported in coagulase-negative staphylococci in 1979 and 1983. From the late 1960s through the early 1980s, the pharmaceutical industry introduced many new antibiotics to solve the resistance problem, but after that the antibiotic pipeline began to dry up and fewer new drugs were introduced (Ventola, 2015).

Among Gram-positive pathogens, a global pandemic of resistant S. aureus and Enterococcus species currently poses the biggest threat. Methicillin-Resistant S. aureus (MRSA) kills more than HIV/AIDS, Parkinson’s disease, emphysema, and homicide combined. Vancomycin-resistant enterococci (VRE) and a growing number of additional pathogens are developing resistance to many common antibiotics. The global spread of drug resistance among common respiratory pathogens, including Streptococcus pneumoniae and Mycobacterium tuberculosis, is epidemic Rossolini et al. (2014).
Gram-negative pathogens are particularly worrisome because they are becoming resistant to nearly all the antibiotic drug options available, creating situations reminiscent of the pre-antibiotic era. The most serious Gram-negative infections occur in health care settings and are most commonly caused by Enterobacteriaceae (mostly Klebsiella pneumoniae), Pseudomonas aeruginosa, and Acinetobacter. Multi-drug resistant gram-negative pathogens are also becoming increasingly prevalent in the community. These include extended-spectrum beta-lactamase-producing Escherichia coli and Neisseria gonorrhoeae. Rossolini et al. (2014).
Causes of Antibiotic Resistance
Although the causes of antibiotic resistance are spontaneous and complex but we cannot preclude human activities at different levels of society. Below are some human activities that influence the development of antibiotic resistance.
1. Irrational use of antibiotics
Misuse/overuse of antibiotics is rampant in both developed and developing countries. Some ailments like common cold do not warrant any antibiotics, yet these are widely prescribed. An epidemiological study had demonstrated a direct relationship between antibiotic consumption and the emergence and dissemination of resistant bacteria strains. The overuse of antibiotics clearly drives the evolution of resistance.
2. Inappropriate prescription
Incorrectly prescribed antibiotics also contribute to the promotion of resistant bacteria. Studies have shown that treatment indication, choice of agent, or duration of antibiotic therapy is incorrect in 30% to 50% of cases. In many instances, especially in the developing countries, antibiotics even when properly prescribed are not well taken by patients, thus providing a favourable condition for resistant bacteria to proliferate (Ventola, 2015).

3. Extensive Agricultural Use
In both the developed and developing world, antibiotics are widely used in agricultural settings. Antibiotics have three uses in agricultural animals: treatment of infection, prevention of infection, and growth promotion. Preventing infection and promoting growth both require widespread distribution of antibiotics to animals, greatly increasing the chance of resistance. Use of antibiotics as growth promoters is controversial and has been prohibited in some European countries. The antibiotics used in livestock are ingested by humans when they consume foods such as meat and milk (Ventola, 2015).
4. Insufficient New Antibiotics
In the past, development of new antibiotics by the pharmaceutical industry was an effective strategy for combating resistant bacteria. This had recently stalled due to economic and regulatory issues. Antibiotic research conducted in academia has been scaled back as a result of funding cuts due to the economic crisis. According to Bartlett et al.(2013) antibiotic development is no longer considered to be an economically wise investment for the pharmaceutical industry. This is because antibiotics are used for relatively short periods and are often curative, antibiotics are not as profitable as drugs that treat chronic conditions, such as diabetes, psychiatric disorders, asthma, or gastroesophageal reflux.
Mechanisms of Antibiotic Resistance
Bacteria have a remarkable genetic makeup that allows them to respond to a wide array of environmental threats, including the presence of antibiotic molecules that may jeopardize their existence. The gene coding for resistance in bacteria can be developed naturally through mutation or acquisition of foreign DNA coding for resistance determinants through horizontal gene transfer Muntia and Arias, (2016).
Generally there are three (3) fundamental mechanisms for resistance in bacteria. They are: modifications of the antibiotic molecule; prevention of the antibiotic from reaching the target; change of target sites
i. Modifications of the Antibiotic Molecule
In the presence of antibiotics, bacteria can produce enzymes that inactivate the drug by adding specific chemical moieties to the compound or that destroy the molecule itself, rendering the antibiotic unable to interact with its target. It is a well-known mechanism of acquired antibiotic resistance in both gram-negative and gram-positive bacteria.
ii. Prevention of the antibiotic from reaching the target
Many of the antibiotics used in clinical practice have intracellular bacterial targets or, in case of gram-negative bacteria, located in the cytoplasmic membrane (the inner membrane). Therefore, the compound must penetrate the outer and/or cytoplasmic membrane in order to exert its antibiotic effect. Bacteria have developed mechanisms to prevent the antibiotic from reaching its intracellular or periplasmic target by decreasing the uptake of the antimicrobial molecule. This mechanism is particularly important in Gram-negative bacteria, limiting the influx of substances from the external milieu.
iii. Changes in Target Sites
Bacteria have evolved different tactics, including protection of the target (avoiding the antibiotic to reach its binding site) and modifications of the target site that result in decreased affinity for the antibiotic molecule.
Prevention of the Spread of Antibiotic Resistance
In order to prevent further spread of antibiotic resistance, the following measures should be made:
Individuals should only use antibiotics when prescribed by medical professionals and if you are prescribed antibiotics always complete the course; never share the drugs or use leftover prescriptions; never demand antibiotics if your doctor says you don’t need them.
Doctors should only prescribe antibiotics when absolutely necessary; report antibiotic-resistant infections to surveillance teams; talk to your patients about how to take antibiotics correctly, antibiotic resistance and the dangers of misuse.
In the agricultural sector, antibiotics should only be given to animals under veterinary supervision; antibiotics should not be used for growth promotion or to prevent diseases in healthy animals; vaccinate animals to reduce the need for antibiotics and use alternatives to antibiotics when available
Health care industry should invest in research and development of new antibiotics, vaccines and diagnostics.

In conclusion, we must recognize that antibiotics are a precious resource for mankind. We all need to work together to preserve and prolong their efficacy through their rational use and by reducing the burden of infectious diseases through all possible means. We cannot, at any cost, allow our world to slide into the dark days of the pre-antibiotic era.
References
Singh, P. K. (2014). Pre-Antibiotic era looming large - The world is almost out of time. Available here
Gould, I.M. and Bal, A.M.v(2013). New antibiotic agents in the pipeline and how they can overcome microbial resistance. Virulence 4(2): 185–191. Available here
Swain, F. (2011). Antibiotic resistance: Bacteria are winning the war. Available here
Bartlett, J.G., Gilbert, D.N. and Spellberg, B. (2013). Seven ways to preserve the miracle of antibiotics. Clinical Infectious Diseases 56(10):1445–1450. Available here
The antibiotic alarm. (2013). Nature. 495(7440):141. Available here
Ventola, C.L. (2015). The antibiotic resistance crisis. Available here
Muntia, J.M. and Arias, C.A. (2016). Mechanisms of antibiotic resistance. Available here
Rossolini, G.M., Arena, F., Pecile, P. and Pollini, S. (2014). Update on the antibiotic resistance crisis. Clinical Opinion on Pharmacology 18: 56–60. Available here

Thank you for reading!
If you write STEM (Science, Technology, Engineering, and Mathematics) related posts, consider joining #steemSTEM on discord here. If you are from Nigeria, you may want to include the #stemng tag in your post. You can visit this blog by @stemng for more details. You can also check this blog post by @steemstem here and this guidelines here for help on how to be a member of @steemstem. Please also check this blog post from @steemstem on proper use of images devoid of copyright issues here


Join us on air-clinic discord channel here