A SAD INTRODUCTION
Despite advancements in technology and healthcare delivery systems in the world, countries in some part of Africa and Asia are still struggling with maternal mortality (death) and the incidence in this age is quite catastrophic and could remain this way for years to come if nothing is done about it. Maternal mortality is the death of a woman while pregnant, or within 42 days of termination of pregnancy. While maternal mortality rate and maternal mortality ratio are often used interchangeably, they, however, don’t have the same meaning. You may want to check here for a better understanding of these terms. For the sake of clarity, I would be referring to maternal mortality ratio (MMR) in this article; which is the number of maternal deaths per 100,000 live births. My country, Nigeria is of particular importance with regards to MMR, and most of my fact findings would come from data obtained in Nigeria.

A group of ever-hopeful African mothers. source
Gestation (the usual 9 months period during pregnancy) and every other activity surrounding it, is seemingly a critical period for the approximately 9.2 million women and girls who become pregnant in Nigeria each year. They face a lifetime risk of maternal death of 1 in 13 women as compared to 1 in 31 for sub-Saharan Africa as a whole, as reported by the African Population and Health Research Center
As of 2017, Nigeria’s estimated annual 40,000 maternal deaths account for about 14% of the global total, the second largest MMR after India. Presently Nigeria has dropped to number 4 compared to India’s 56th rank. Although MMRs have declined considerably on a global scale since 1990, the pace reduction has been much slower in Nigeria compared to the rest of the world. See the figure below.
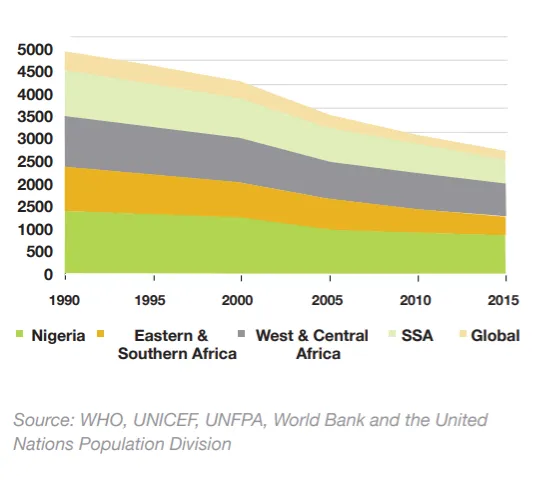
Trends in maternal mortality (per 100,000 live births): 1990 to 2015. source
CAUSES OF MATERNAL DEATHS
The most common cause of maternal death in Nigeria that pushes up the MMR is heavy bleeding following delivery(postpartum haemorrhage) which accounts for 23% of all maternal deaths. This is followed by infections following childbirth (sepsis) at 17%. Unsafe abortion is another leading cause of maternal death in Nigeria (11%), but this is a story for another day.
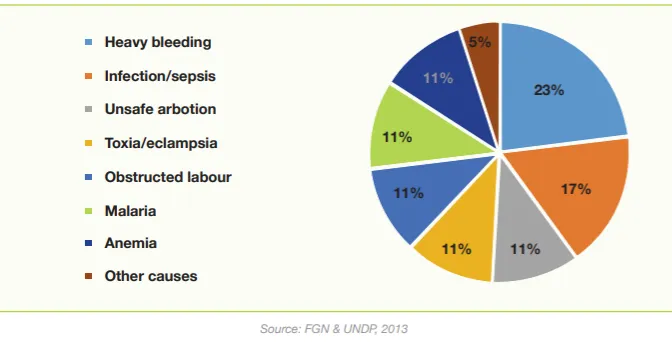
Causes of maternal deaths as a percentage of the total, Nigeria, 2013 source
It is important to note that these 3 important causes are linked to (a significant percentage) employing the services of unqualified persons in health care delivery. Hopefully, maternal mortality would someday be a thing of the past as the United Nations (UN) through the World Health Organisation (WHO) has been partnering with health-related bodies and positively affected third world countries to combat this plague in line with her Millennium Development Goals.
The MDGs at a glance 
source: Wikimedia Commons By Kjerish - Own work, CC BY-SA 4.0.
CARBETOCIN TO THE RESCUE:
Since the major cause of MMR is postpartum haemorrhage (PPH), it is only logical that better or improved measures to arrest bleeding after delivery should be sought after. Recently, an Investigational New Drug (IND), carbetocin has been endorsed to not only give comparable results with oxytocin (which is currently used for the treatment of PPH) but is also thermostable (relatively not destroyed or inactivated by heat)!
Now she can smile to the labour ward source
Currently, the WHO recommends oxytocin as the first-choice (standard) drug for the treatment of PPH, but the problem with oxytocin is that it requires cold storage (refrigeration). The drug must be stored and transported at 2 to 8-degree Celsius, which is hard to achieve in low-and lower-middle income countries. This denies women in these countries access to this life-saving drug and even when available, most times, the drug is less effective because it has been exposed to heat. A survey carried out in 2016 showed that 74.2% of oxytocin samples in Nigeria failed laboratory quality evaluations.
The clinical trial studied close to 30,000 women who gave birth vaginally in 10 countries: Argentina, Egypt, India, Kenya, Nigeria, Singapore, South Africa, Thailand, Uganda and The United Kingdom. Each woman was randomly given a single injection of carbetocin or oxytocin immediately after birth and the study found that both drugs were equally effective at preventing excessive bleeding after delivery.
The results achieved were promising as carbetocin is not only as effective but also as safe as oxytocin in the prevention and treatment of PPH. The formulation does not require refrigeration and retains its efficacy for at least 3 years stored at 30-degree Celsius and 75% relative humidity. Truly, a breath of fresh air!

Truly a breath of fresh air! source
AWAY WITH OXYTOCIN?
Following this great discovery, the next step is regulatory review and approval by drug agencies of countries. While the WHO is considering making carbetocin the drug of choice for the prevention and treatment of PPH, the authorities of countries affected should make provisions for effective storage and delivery of oxytocin. Provision of stable electricity and cooling systems is of utmost importance. Maybe a time will come when oxytocin would no longer be the drug of choice, but no doubt, it has played a vital role in saving millions of lives. Do you think regulatory authorities should focus on endorsing carbetocin, phasing out oxytocin or improving conditions for the effective delivery of oxytocin?

carbetocin or oxytocin?. modified by Michael, my brother.
Thanks for reading. I hope you learnt something.
You may want to know more About me.
I represent @steemSTEM and @stemng
REFERENCES
African Population and Health Research Center
https://data.unicef.org/topic/maternal-health/maternal-mortality/#
https://en.wikipedia.org/wiki/Millennium_Development_Goals
https://www.indexmundi.com/g/r.aspx?c=ni&v=2223
FURTHER READING