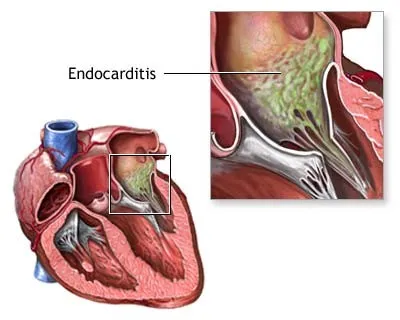
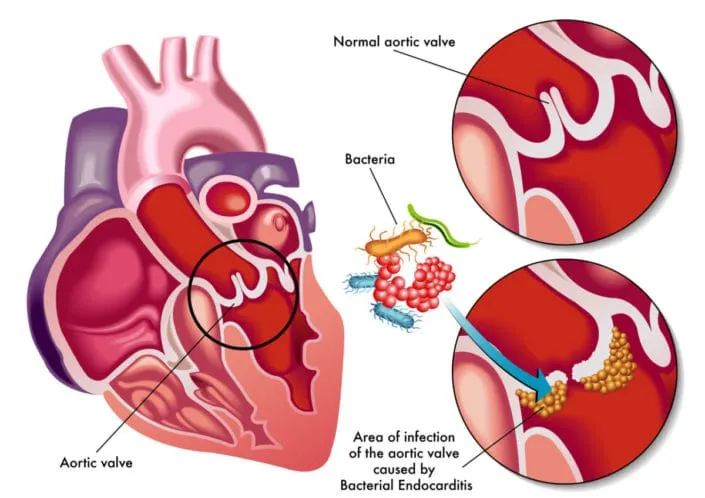
Infective endocarditis (IE), also known as bacterial endocarditis, is the inflammation of endothelial layer of heart. It is a very serious heart disease which is sometimes very difficult to diagnose and treat associated with high mortality and severe complications. IE is caused by bacteria that enter the bloodstream and settle in the heart lining, a heart valve or a blood vessel. It may also be developed on devices implanted in the heart, for example: artificial heart valves, pacemakers or implantable defibrillators. When normal blood components, like fibrin and platelets, stick to the bacteria, the resulting build-up is called a vegetation.
How Infective Endocarditis Affects Us?
Endocarditis can limit the heart’s ability to efficiently pump blood. Damaged infected valves can cause severe leaking (regurgitation) of blood back through the valve(s). Small pieces of vegetation can break off and travel through the blood vessels to other parts of the body and caused problems like stroke or tissue damage.
Symptoms
General signs of infection include fever, chills and leukocytosis (sudden increase in white blood cells) which can leads to sepsis. When vegetation breaks off, it can create emboli. If emboli breaks off and go to right-sided valves or chambers, it can cause lung pulmonary embolism; if it go to left sided valves or chambers, it might cause blockage in brain, kidney or spleen.
Risk factors
- An artificial (prosthetic) heart valve
- Heart valves repaired with artificial material
- History of endocarditis
- Congenital heart defects
- Abnormalities of the heart valves resulting from heart transplantation
- History of intravenous illegal drug use
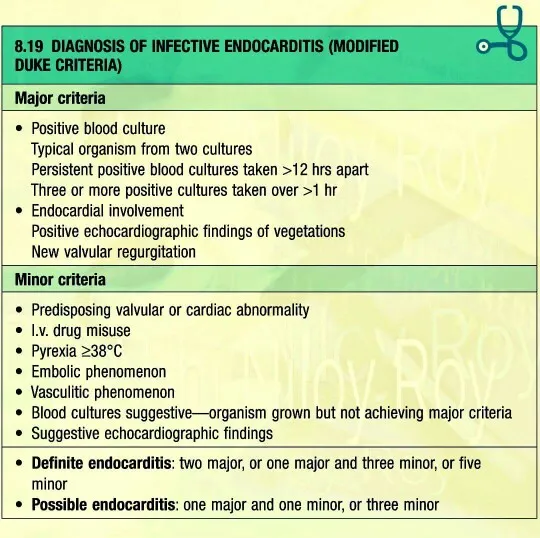
Diagnosis of IE requires of multiple clinical, laboratory, imaging findings. Blood cultures should be incubated for a minimum of 7 days, which should result in a positive culture for 95% of IE cases. Duke criteria use a set of major and minor clinical and pathologic criteria to classify infectious endocarditis as definite, possible or rejected.
Goals of therapy
- Eradicate infection
- Treat sequelae of destructive intra-cardiac and extra-cardiac lesions
The choice and duration of treatment depend upon:
- the type of microorganism and its susceptibility profile
- allergy to antimicrobials
- whether infection involves a native and prosthetic valve
Treatment of IE should be tailored to etiologic agent.
- Common blood culture isolates include Staphylococcus aureus, streptococcus, enterococci and coagulase-negative staphylococci.
Effective antimicrobial treatment should lead to defervescence within 7-10 days.
If structural and functional integrity of cardiac valves damaged by infection, it may lead to valvular regurgitation or flow obstruction in valves with large vegetations. Hence, surgical intervention is warranted for valve dehiscence, perforation, rupture or fistula, or a large perivalvular abscess.