Hi Everyone,

Many countries around the world are currently suffering from some sort of health crisis. The responses to Covid-19 have greatly contributed to these crises (see my post Covid-19 Crimes and Vaccine Fraud). The number of excess deaths has increased, the number of people that have taken time off work because of illness has increased, the extent of chronic illness has increased, waiting times for medical procedures have increased, and response times to emergencies have increased. Even without the events of Covid-19, our health systems were not performing as well as they should. This appears to be design rather failed genuine attempts to improve healthcare and health.
I have posted about health a couple of times. In my post, Health - Dark Side of Economics, I discussed how health systems have failed us because it is in the interest for Governments (e.g. justify higher expenditure) and large pharmaceutical companies (e.g. obtain higher and sustained profits). In my post, Health - Prevent, Cure, or Treat, I discussed how increased Government expenditure on health has not, in general, improved health outcomes. I also discussed the strong focus on treatment rather than prevention or cure. In this post, I discuss, with the support of data, why the healthcare systems are failing and how systems can be improved so that we can reach our desired health outcomes.
Current Decline in Health and Healthcare
Despite the problems with the healthcare systems, life expectancy, for almost every country in the world, has consistently increased throughout recorded history. Since 2020, that has changed. Life expectancy has fallen across the world. For some countries this drop has been large. For example, the life expectancy in the USA dropped from 79.1 years in 2019 to 77.2 years in 2021; this reduces it to what it was in 2003. Figure 1 contains life expectancy trends for continents, least developed, less developed, and most developed countries as well as for large countries such as USA, China, Japan, and India.
Figure 1: Life Expectancy for continents and selected countries (1980 to 2021)
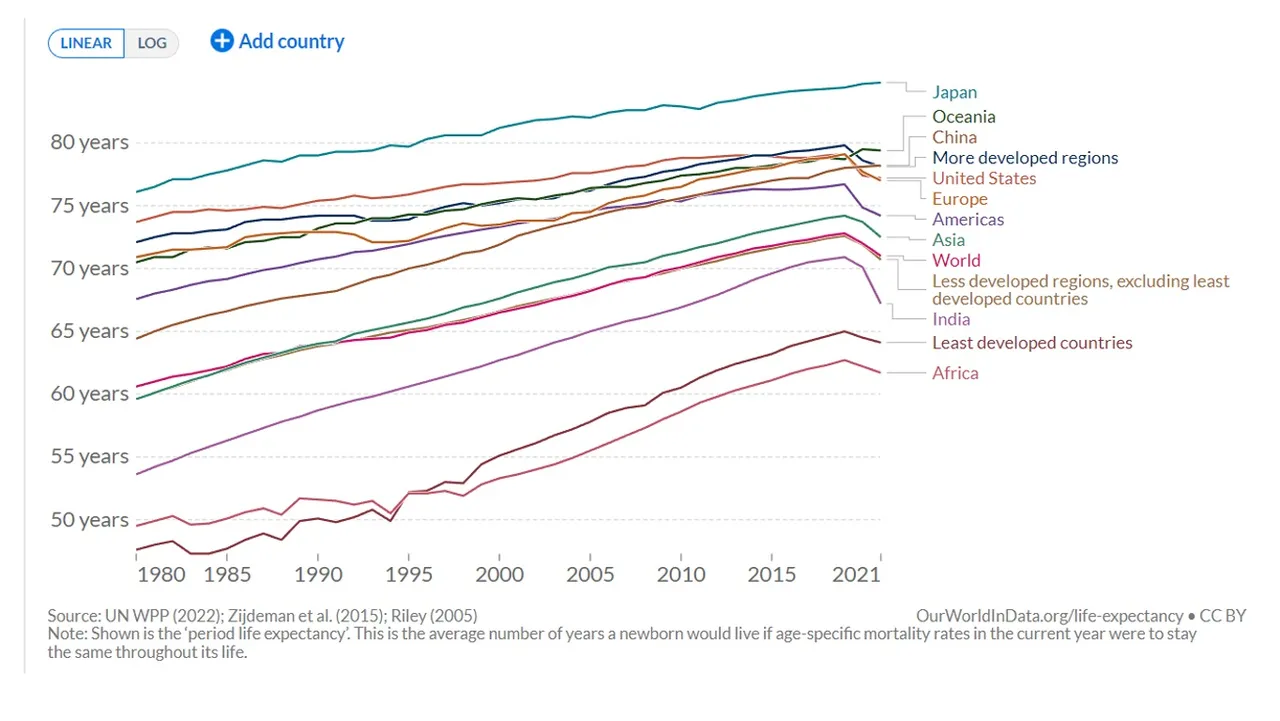
Source: Our World in Data
We could argue that the decline is linked to Covid-19. The highest death toll was amongst the elderly. This could only be used to explain the fall in life expectancy in countries most effected by Covid-19. However, the reduction appears far more widespread and appears to be affecting countries that did not record many Covid-19 related deaths.
Let us consider the number of excess deaths around the world since 2020. Figure 2 contains a map comparing the cumulative number of excess deaths from January 2020 to the beginning of 2023 with the projected number of deaths for the same period based on previous years. Figure 3 contains the trend for cumulative deaths for a few selected countries.
Figure 2: World Map of Cumulative Excess Deaths per million people (from January 2020 to February 2023)
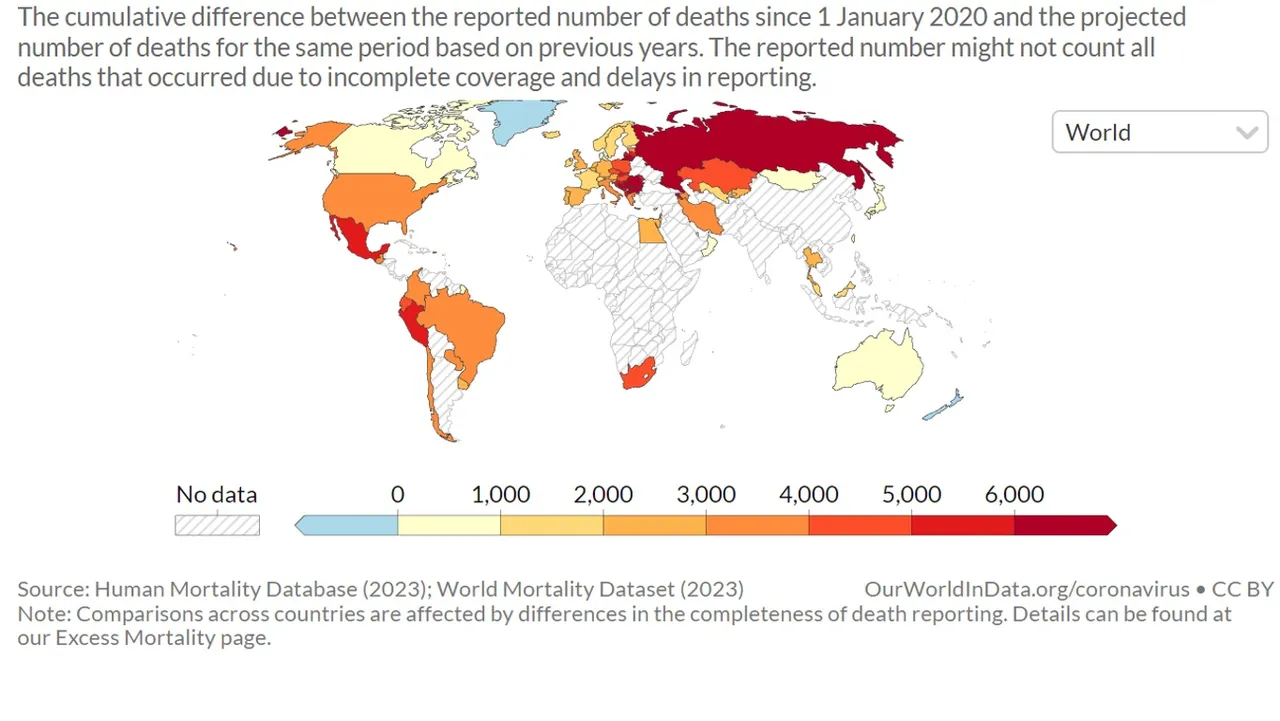
Source: Our World in Data
Figure 3: Cumulative Excess Deaths per million people (from January 2020 to February 2023) for selected countries
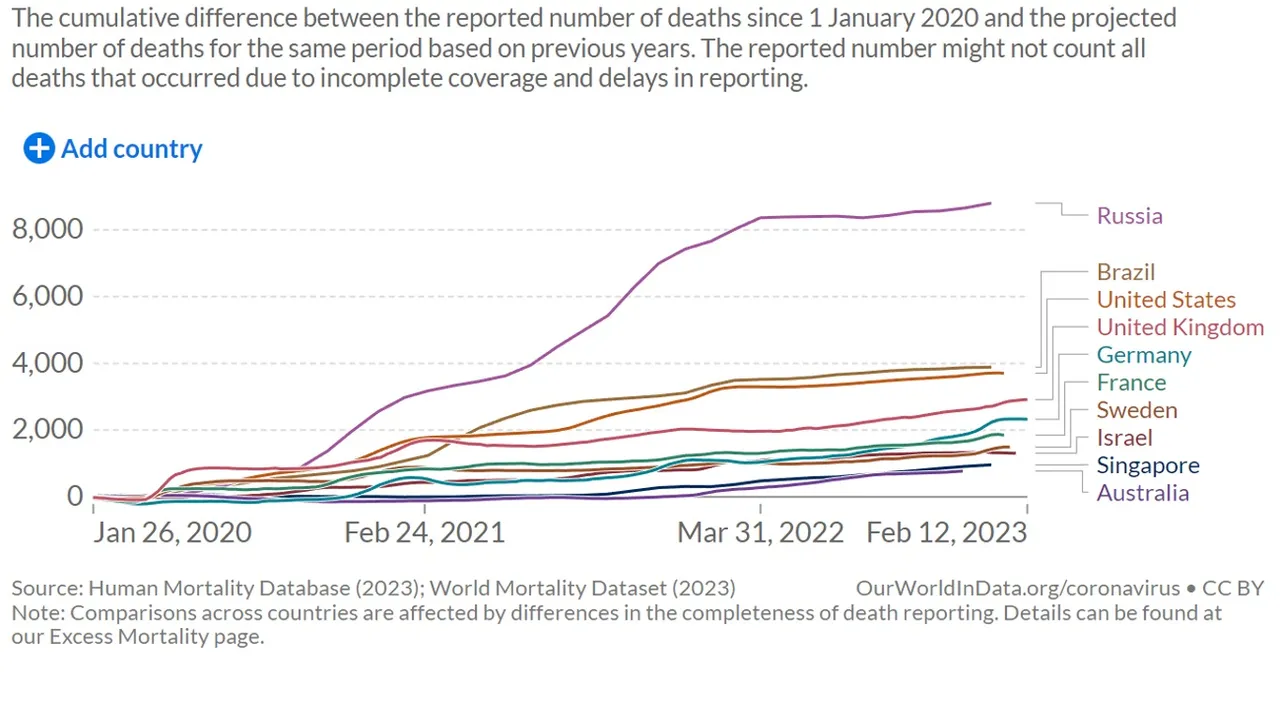
Source: Our World in Data
The world map reveals that excess deaths have increased almost everywhere where data is available. The countries coloured in dark red have performed the worst with cumulative excess deaths exceeding 6,000 per million people. Figure 3 shows how the excess deaths have progressed over this three year period for a few selected countries. It appears excess deaths have continued to increase after the proclaimed pandemic period; this increase is at a decreasing rate for most of the worst affected countries. The pattern in Asia appears a little different. Figure 4 contains the trend in excess deaths in Asian countries with available data.
Figure 4: Cumulative Excess Deaths per million people (from January 2020 to February 2023) for Asian countries
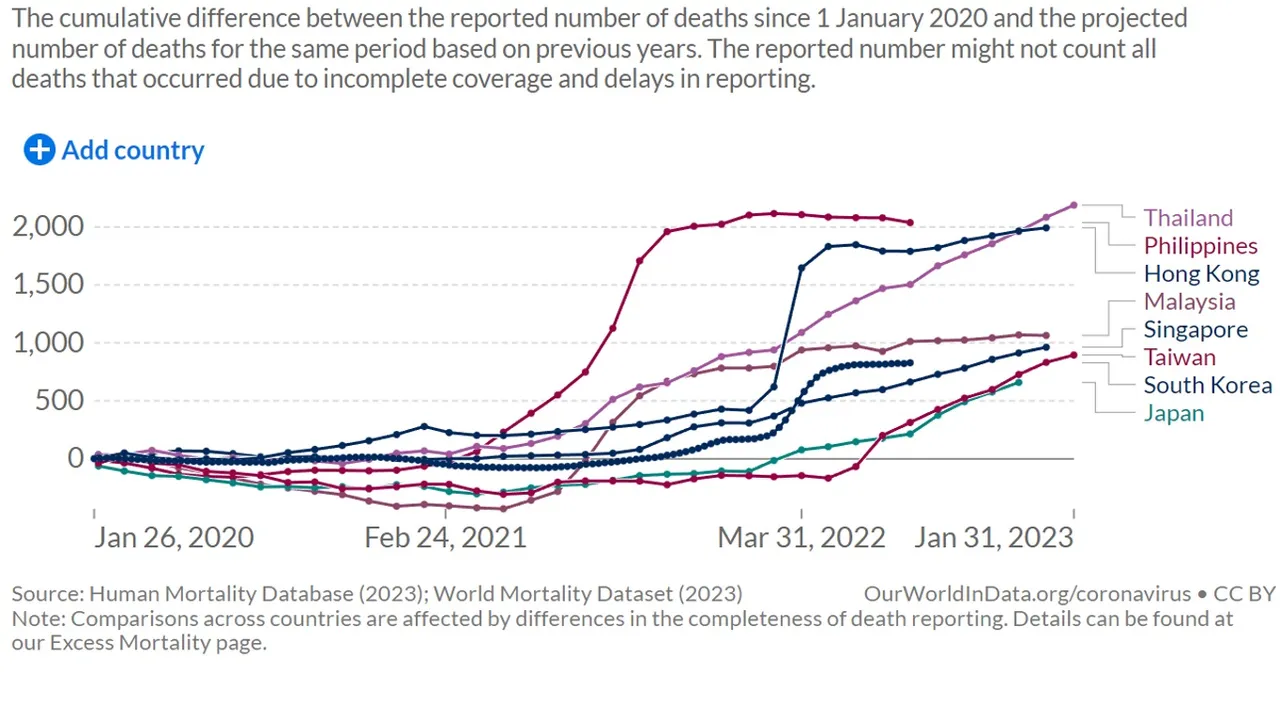
Source: Our World in Data
For 2020 and the first quarter of 2021, excess deaths appeared low and even negative for several of these countries. For the remaining 9 months of 2021, several countries experienced spikes in deaths (e.g. Philippines, Hong Kong, and Malaysia). The other countries are experiencing a continuous increase in the number of excess deaths through until the end of the data range (February 2023).
Falling life expectancy and excess deaths are not the only signs of declining health. Data from the UK indicates that more people are suffering from long term sickness. This can be seen by the increase in the percentage of absenteeism in the workplace. The percentage of absenteeism had been consistent from 2009 to 2019. In 2020, it increased due to larger spikes in the winter. In 2021, it increased throughout the year and continued to increase in 2022, see Figure 5.
Figure 5: Percentage Monthly Sickness Absence rates by NHS England (April 2009 to October 2022)
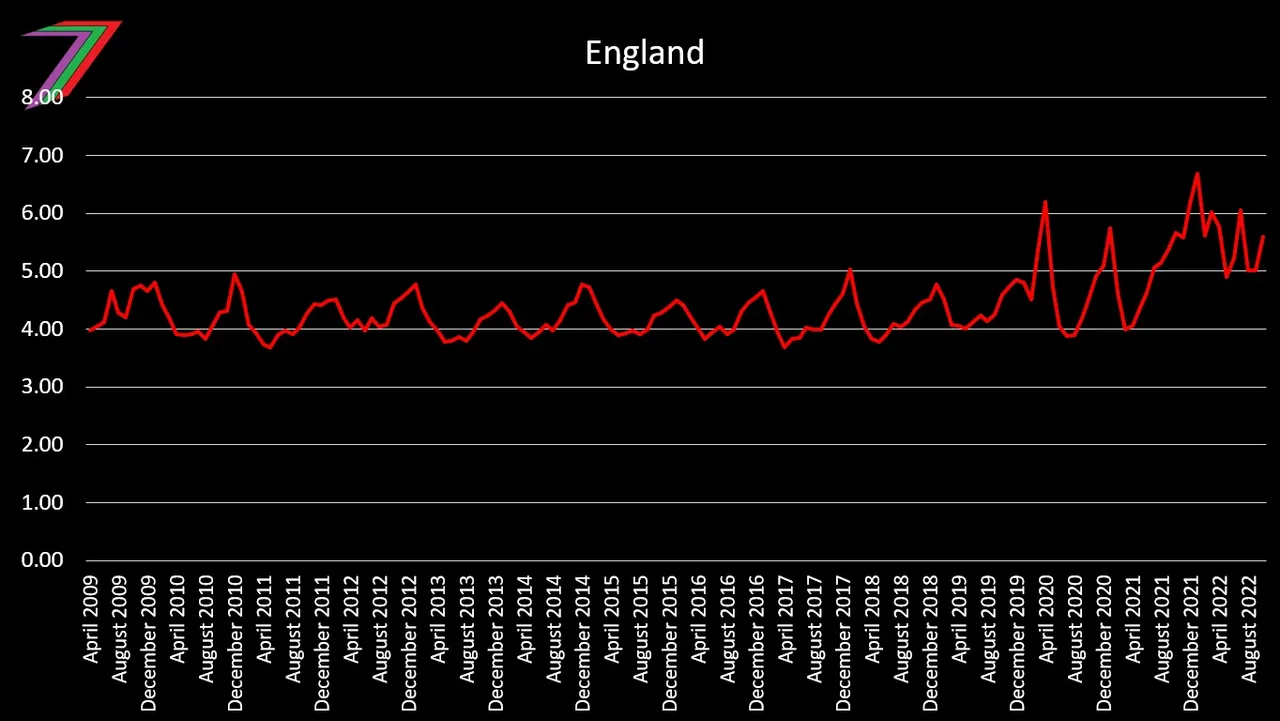
Source: Digital NHS
The number of people becoming economically inactive (deemed themselves unable to work full working hours) because of long term illness has been continuously increasing since the beginning of 2019 with the most rapid increase occurring in 2022. See Figure 6.
Figure 6: Cumulative change in number of people aged 16 to 64 years inactive owing to long-term sickness, seasonally adjusted, UK, January to March 2017 to June to August 2022
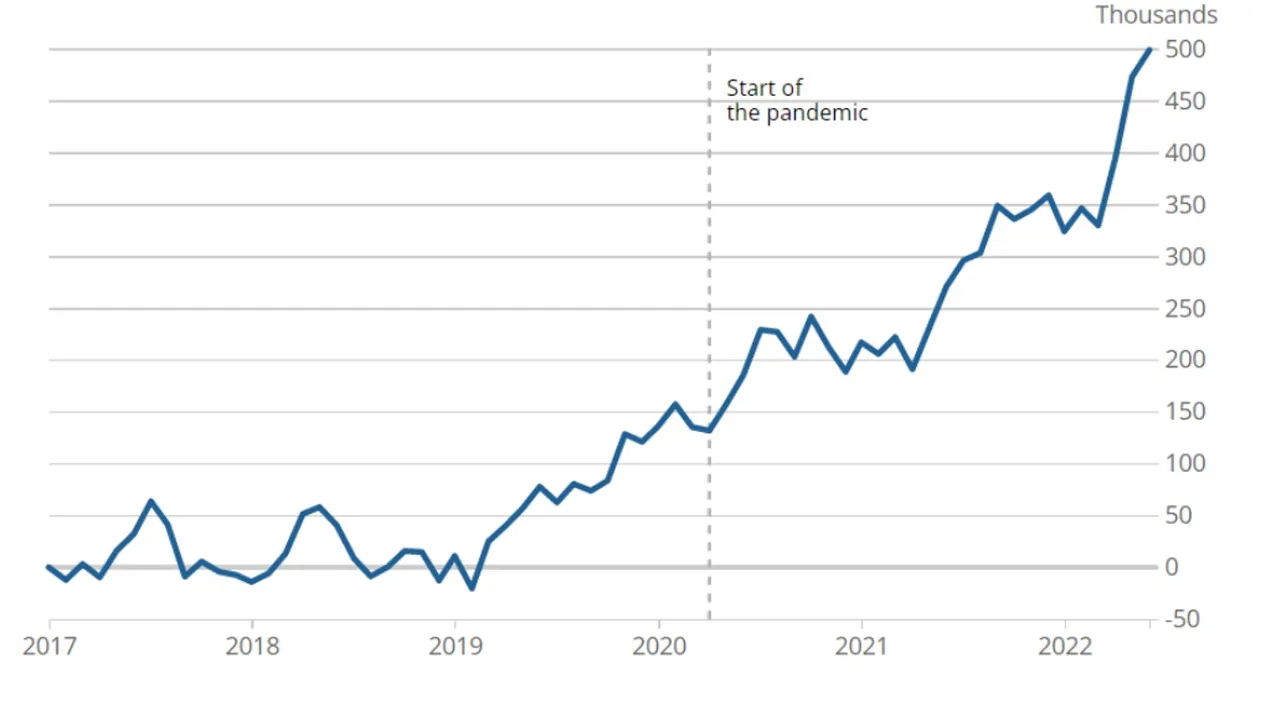
Source: Office for National Statitics
In the UK, waiting times to receive medical attention in the Accident and Emergency Department has been continuously increasing since at least 2015. However, these wait times increased considerably in both 2021 and 2022. This can be seen by the increase in the number of people waiting 12 or more hours to receive medical attention in the Accident and Emergency Departments in hospitals in England, see Figure 7.
Figure 7: Number of patients who waited twelve hours or more in Accident and Emergency Departments in England from 2015 to 2022
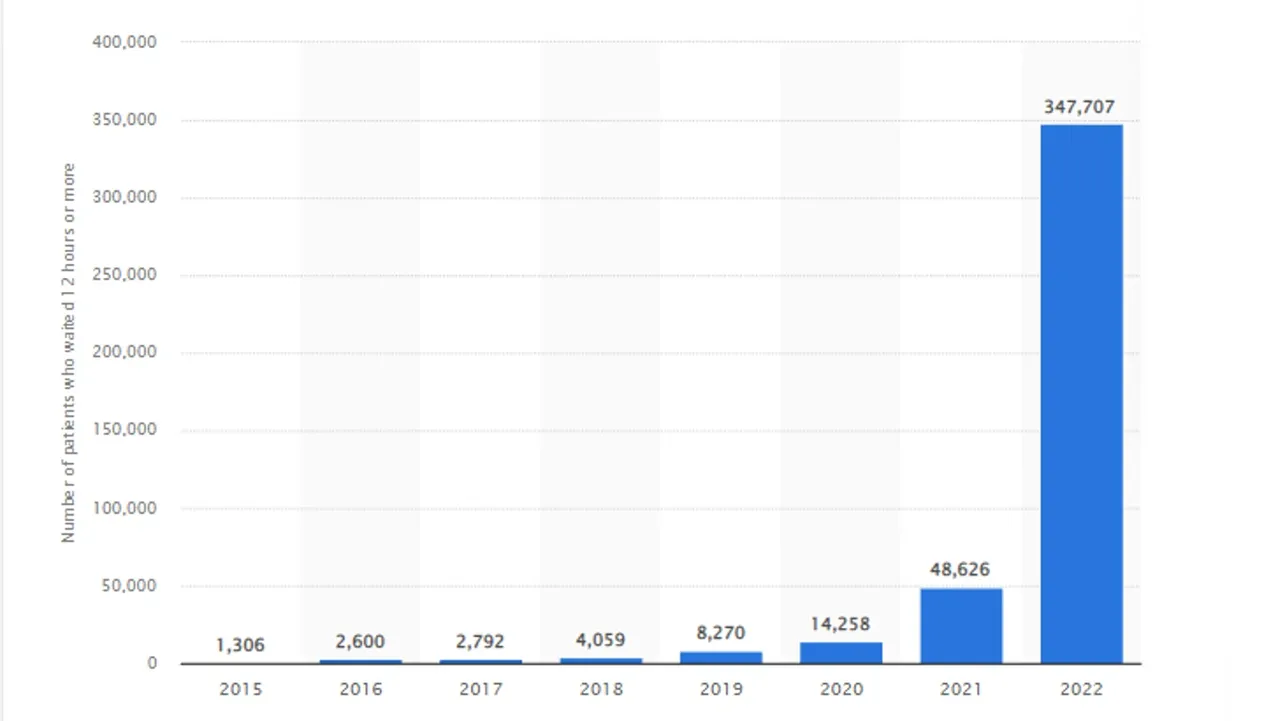
Source: Statista
The UK, England in particularly, have been focused on because of the availability of data. Other countries are having similar problems with declining healthcare and healthcare provision. Figure 8 contains the percentage of people waiting more than a day to see doctors and the percentage of people waiting more than a month to see specialists for selected countries where data is available.
Figure 8: Waiting times for appointments for selected countries (2023)
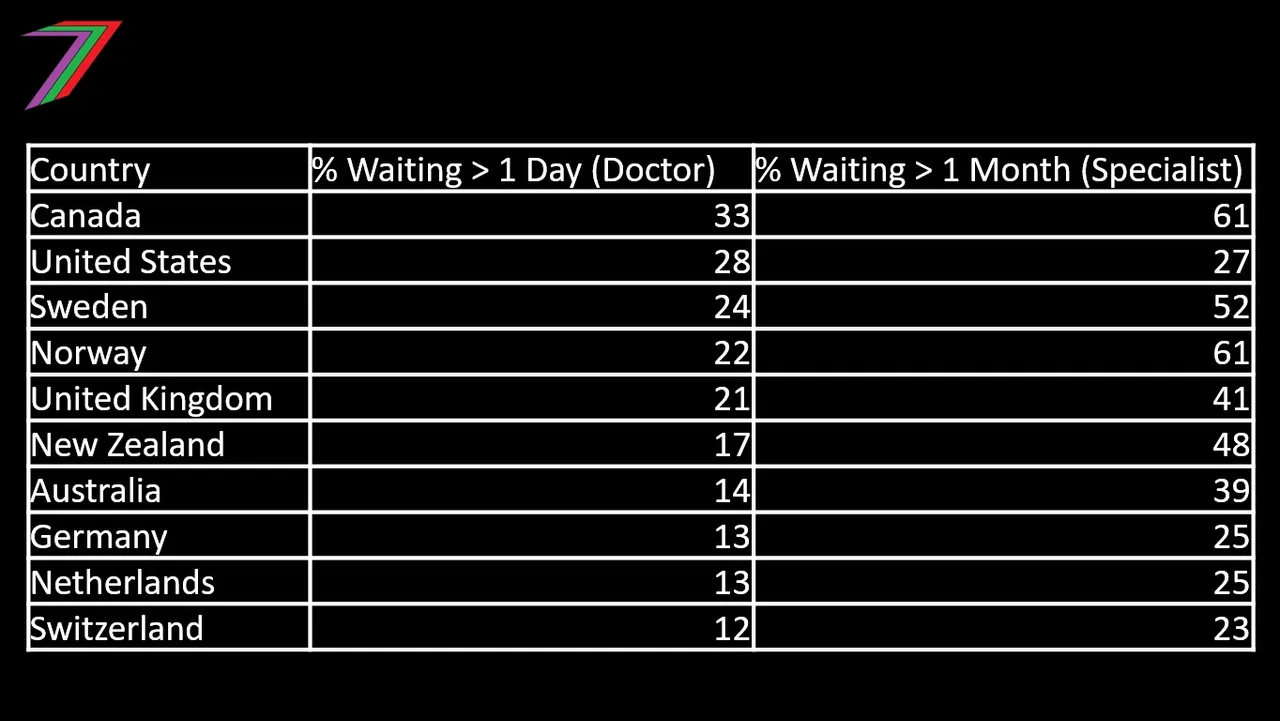
Source: World Population Review
Healthcare has been inadequate for a long time
People’s health and quality of healthcare has declined significantly over the past three years but it was not good before then. Based on 2019 data, approximately 40% of the UK population suffered from at least one chronic health condition (Office for National Statistics). Based on 2017 data, approximately 60% of the US population suffered from at least one chronic health condition and approximately 42% suffered from multiple chronic health conditions (Rand). The number of people on waiting lists in the UK has consistently increased since 2009. See Figure 9.
Figure 9: Number of Patients waiting for NHS hospital treatment in England
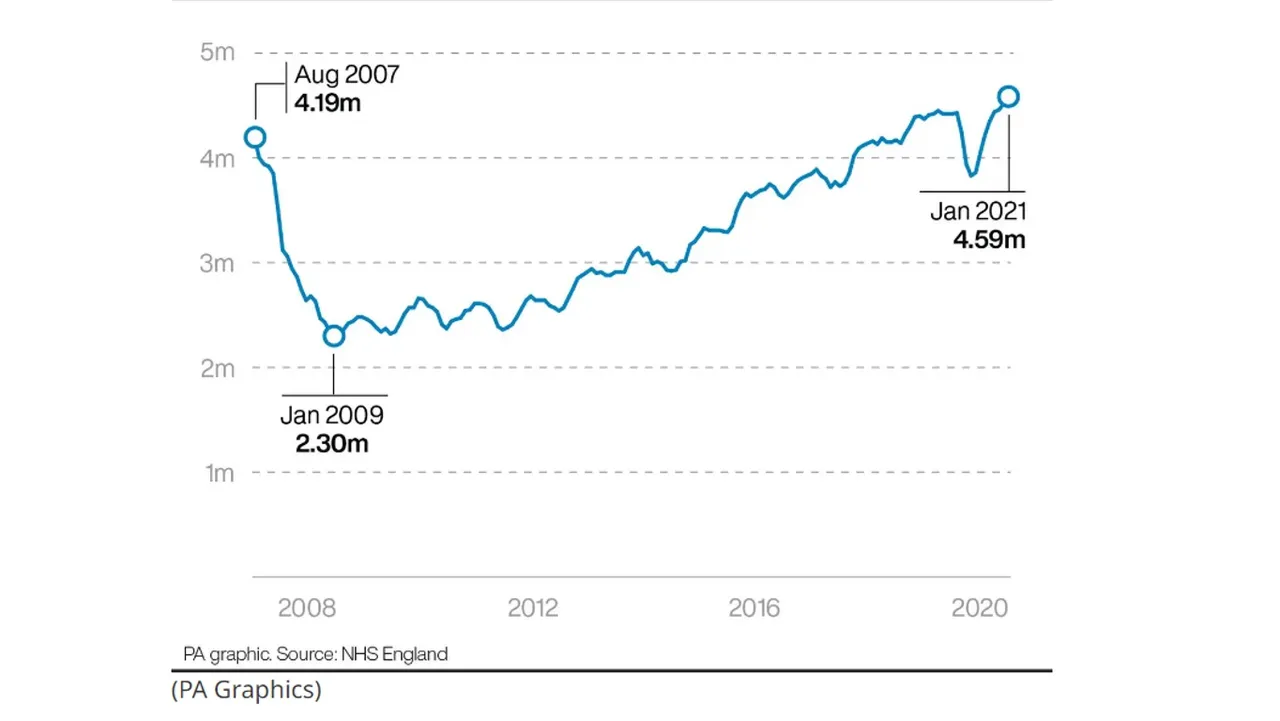
Source: NHS England cited by Lancashire Telegraph
Population Growth and Healthcare
Global population is increasing but at decreasing rate. Eventually, the global population will stop growing and is likely to decline. This is because birth and fertility rates are falling. This decline is occurring across the world. The current fall first became prevalent in developed countries and more recently least developed countries. Figure 10 contains the fertility rates for the world, least developed countries, less developed countries, and more developed countries.
Figure 10: Fertility Rate: Children per Woman (1950 to 2021)
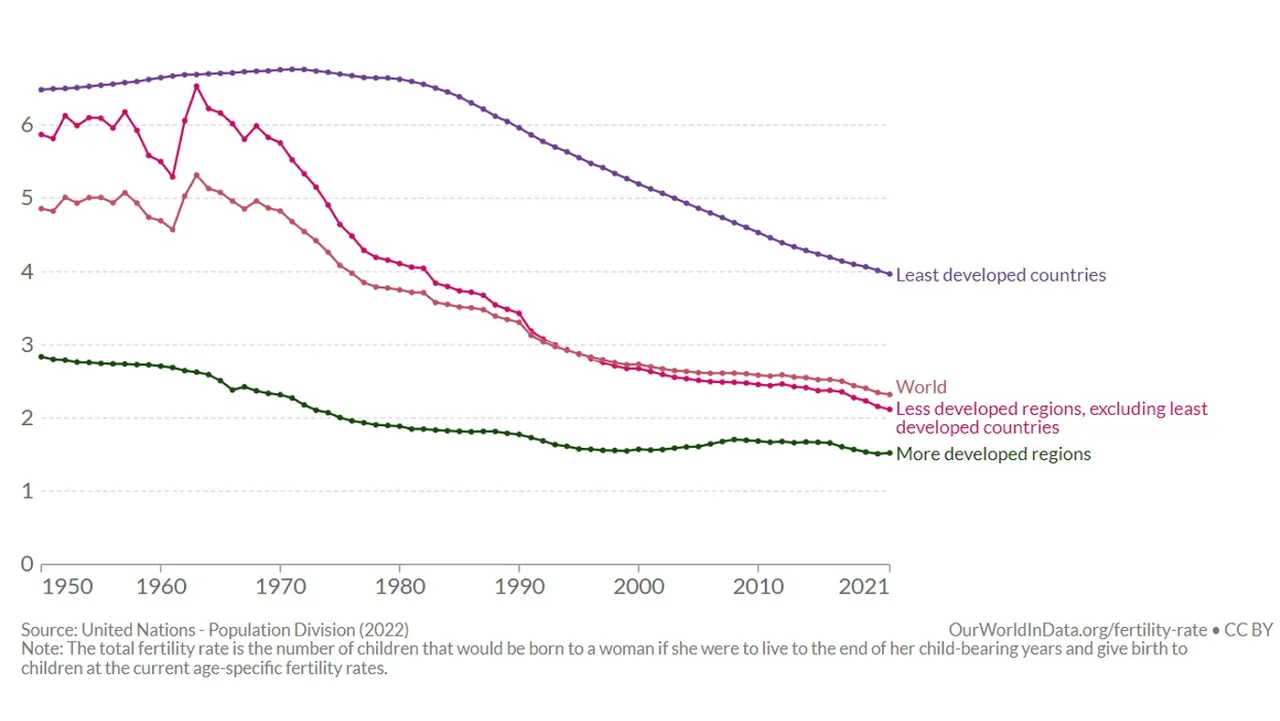
Source: Our World in Data
Many argue that our global population has grown too large. A commonly used argument is that there are too many people competing over the planet’s limited and scarce resources; therefore, causing shortages. The current size of the global population has not caused unavoidable scarcity. Most scarcity is contrived (see my post Scarcity (Part 2) - Natural or Contrived). The concern should not be around the size of the population but the extent of change and the causes of that change. Rapid increases or decreases in population are both bad. Rapid increases leads to shortages because we are unable to adapt to the rapid growth. Rapid decreases leads to gaps in the functioning of an economy; thus, causing it to slow down or even collapse. Rapid decrease in fertility causes the countries age demographic to shift to older people. Older people require more care and healthcare and there are less young people to attend to them. Falling population because of decrease standard of health is bad as our life expectancy and quality of life is reduced.
From a macro perspective, a reasonably stable global population is good. However, it is more important that national and community populations remain reasonably stable. Small increases can be addressed through increased infrastructure and improvements in technology. Small decreases can be addressed through gradual adjustments. Developed countries have had birth rates below the population replacement rate of 2.1 since the early 1970s. This will eventually cause the population of these countries to fall. See Figure 11 for annual change in population for more developed countries.
Figure 11: Population Growth Rate with and without Migration for Developed Countries (1950 to 2021)
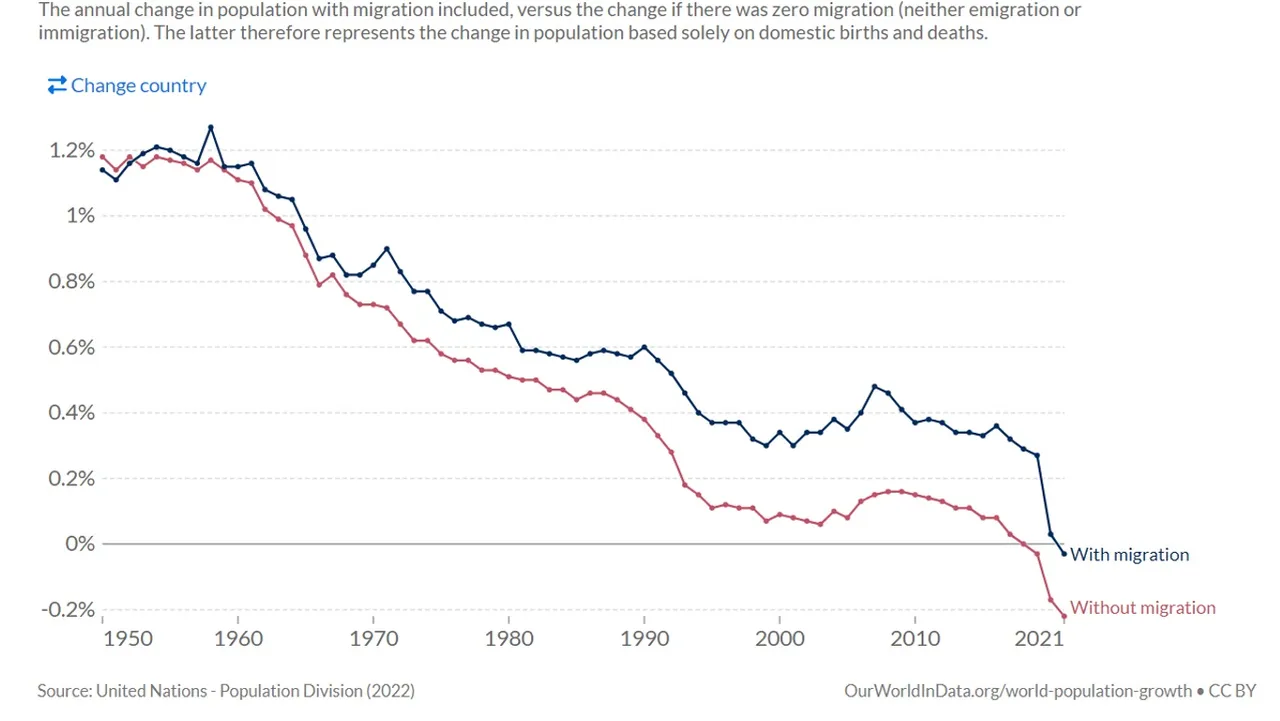
Source: Our World in Data
Net migration can partially offset this decrease but replacement through immigration is not a long term solution for maintaining population levels. Net migration on a global scale is zero. Net migration for some countries will be negative; thus causing populations to fall even faster.
Spending on Healthcare
Global spending on healthcare has been consistently increasing, at least, since the beginning of the new millennium. Figure 12 contains world spending on healthcare from 2000 to 2019.
Figure 12: Health expenditure as percentage of GDP
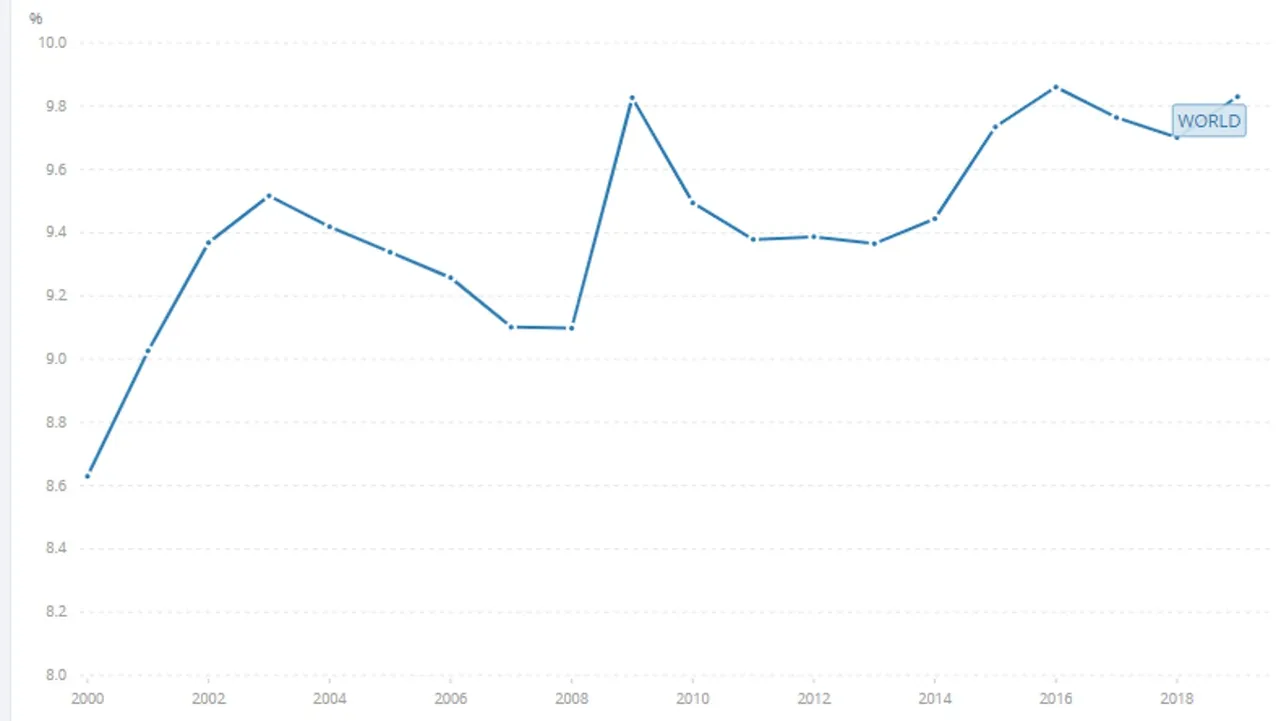
Source: World Bank
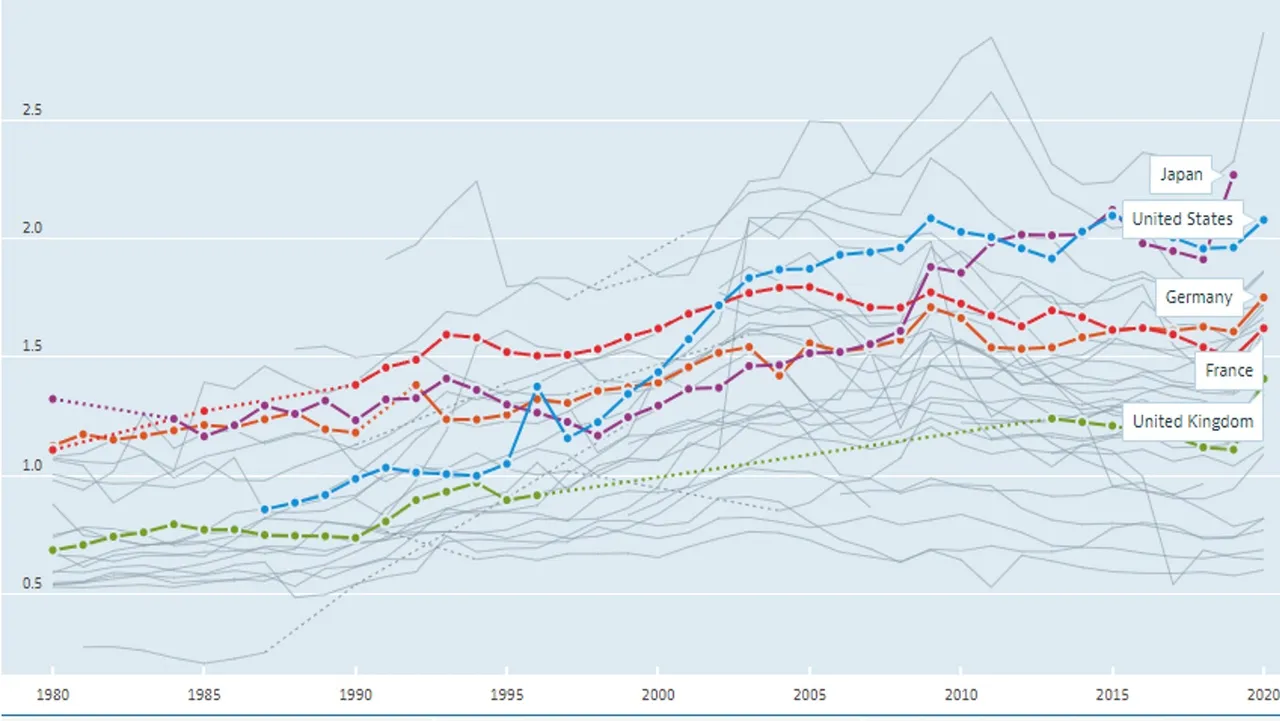
Government spending on healthcare has been consistently increasing for almost all developed countries. Figure 13 contains Government expenditure on healthcare as a percentage of GDP for a few selected developed countries from 1980 to 2021.
Figure 13: Government Health Expenditure as a percentage of GDP (1980 to 2021)
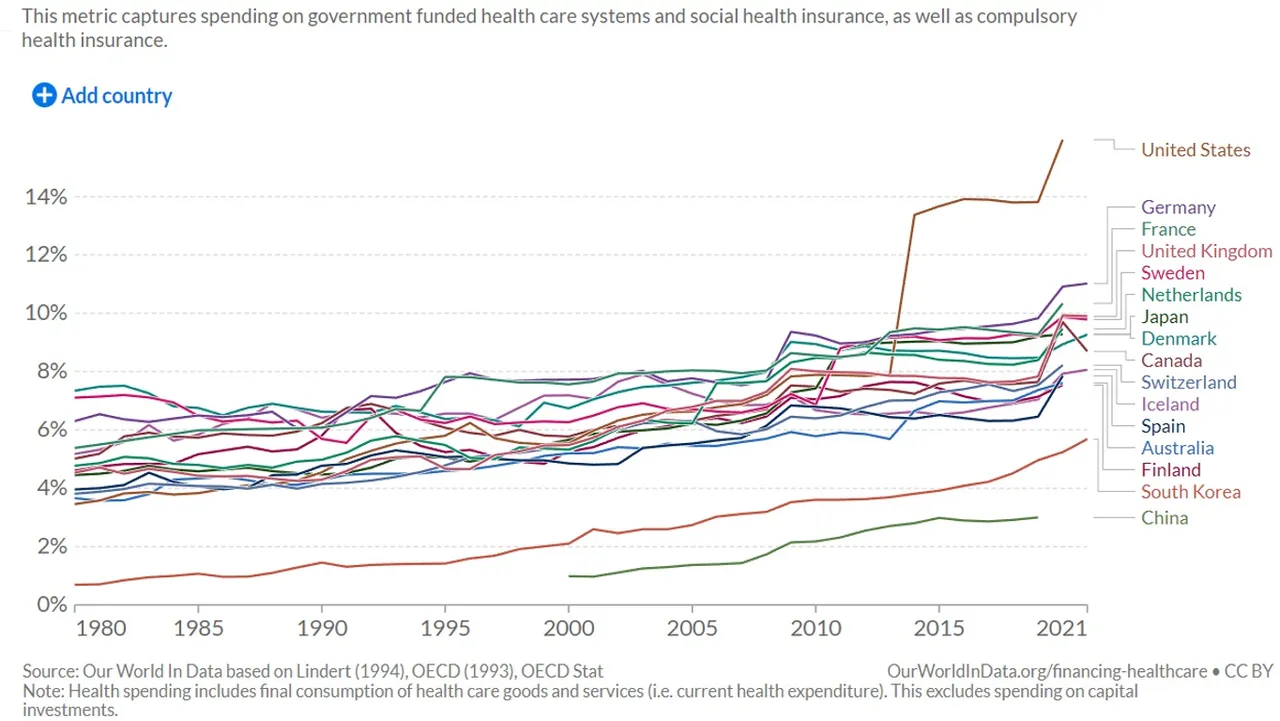
Source: Our World in Data
Increased expenditure on healthcare should lead to improved healthcare and improved health. There is a strong correlation between expenditure on healthcare and life expectancy. Both expenditure on healthcare and life expectancy have trended upwards over time. We could also compare expenditure on healthcare and life expectancy for different countries. See Figure 14.
Figure 14: Life Expectancy vs. Healthcare Expenditure (2000 to 2019 for selected countries)
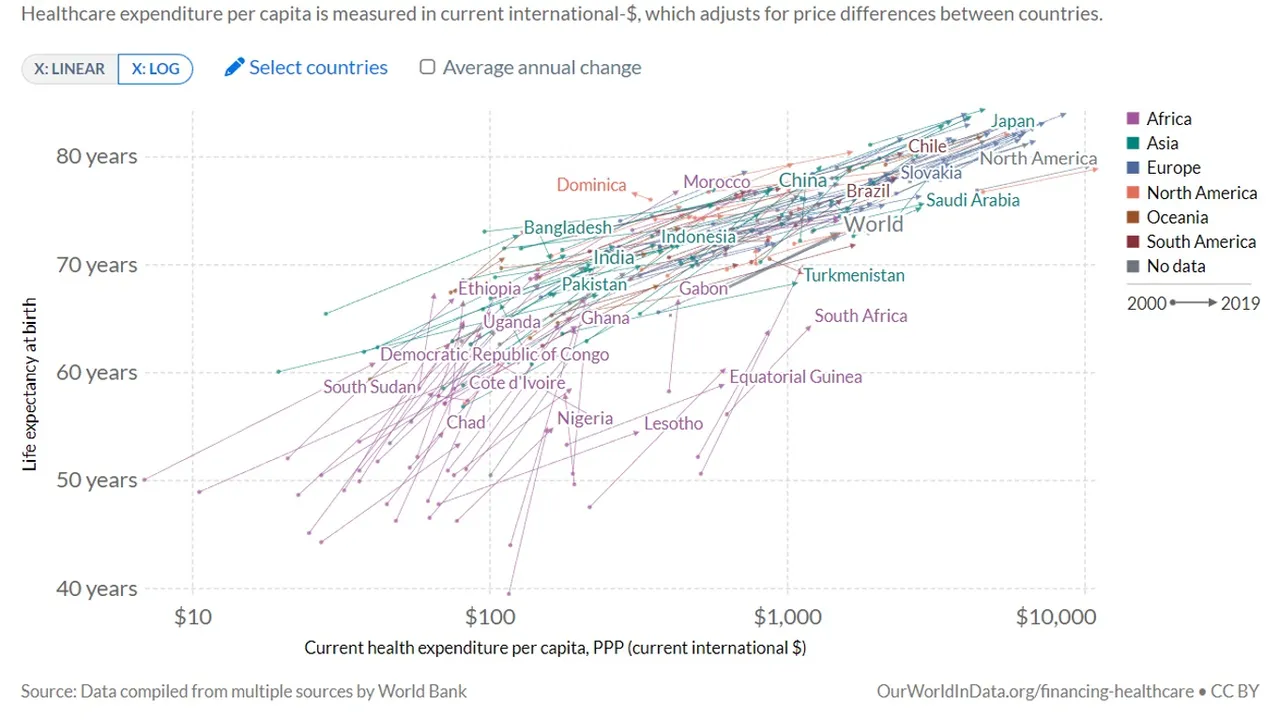
Source: Our World in Data
Figure 14 shows the same correlation between healthcare expenditure and life expectancy over both time and space (i.e. between countries). Correlation does not equate causation. We could draw the same conclusion about the relationship between GDP per capita and life expectancy. Figure 15 contains the relationship between GDP per capita and life expectancy for most of the countries shown in Figure 14.
Figure 15: Life Expectancy vs. GDP per capita (2018)
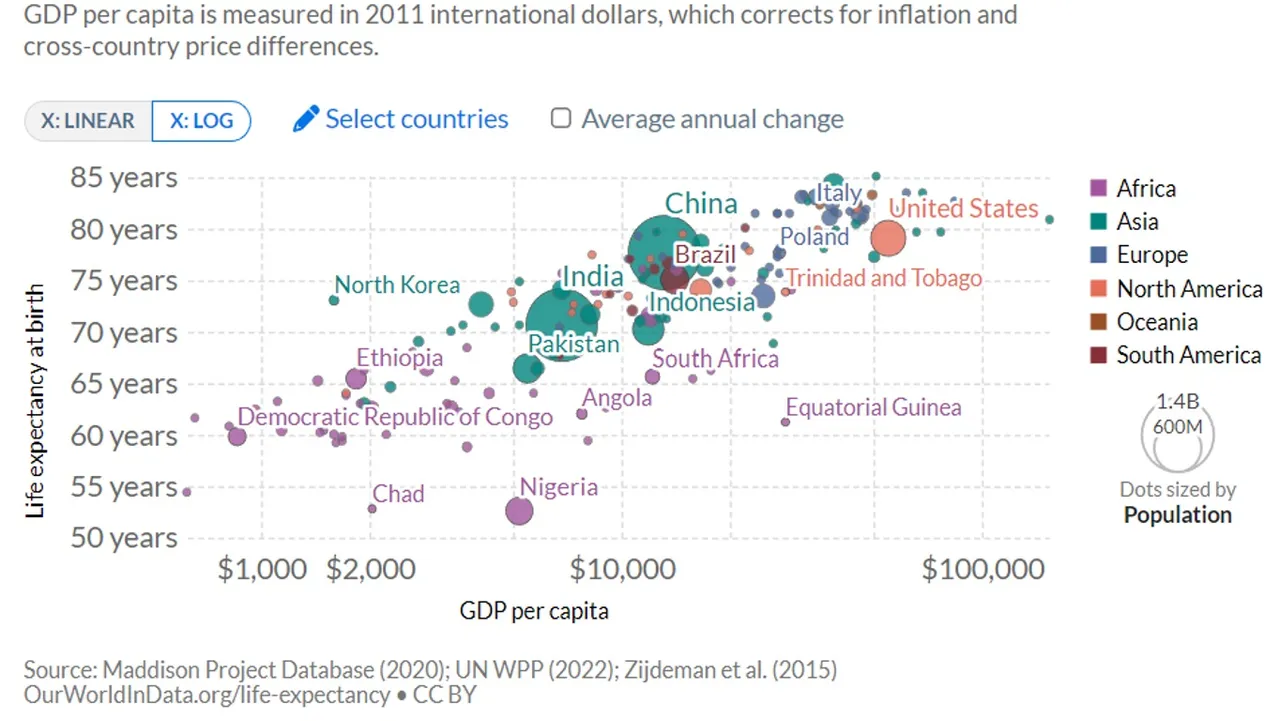
Source: Our World in Data
People in different countries live longer lives for many possible reasons. Many of those reasons are likely related to higher incomes and wealth. Higher GDP also enables higher expenditure on healthcare. This a stronger argument of causation (will revisit this discussion later in the post).
Life expectancy is not the only measurement of better health. Reduced illness is an indication of better health. People could live long lives but the quality of life could be low if they are often ill. As mentioned earlier in the post, people are suffering from more chronic illness and becoming more dependent on medication to treat their illness. Figure 16 contains pharmaceutical spending per capita in US dollars and Figure 17 contains pharmaceutical spending as a percentage of GDP for selected countries.
Figure 16: Pharmaceutical spending per capita in USD for selected countries (1980 to 2020)
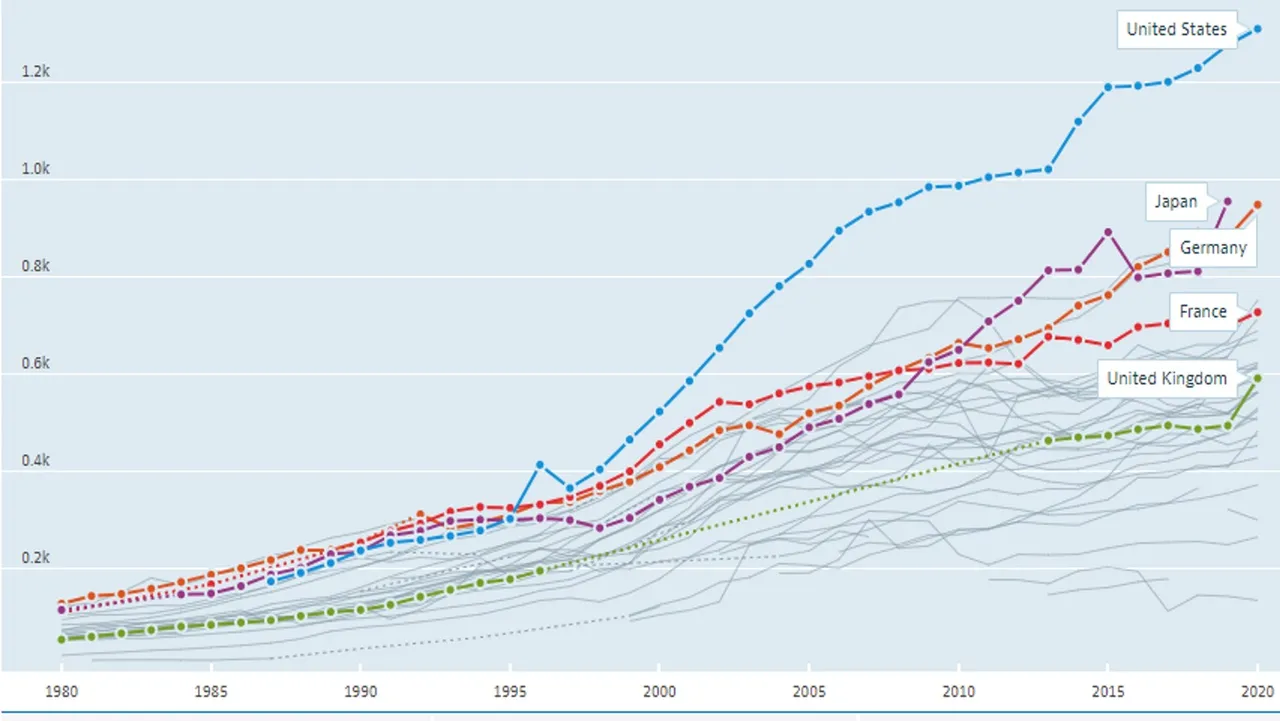
Source: OECD Data
Figure 17: Pharmaceutical spending as percentage of GDP for selected countries (1980 to 2020)
Source: OECD Data
Both figures show large and consistently increasing expenditure on pharmaceutical products for all selected countries as well as all other countries with available data (see greyed out lines). The increasing expenditure plus the percentages of people using pharmaceutical products indicates both dependence on these products as well as their ineffectiveness in curing illness. This is because pharmaceutical companies are focused on treatments instead of cures. Treatments are more profitable because their patients will always need them. These treatments could be a reason why people are living longer. Pharmaceutical companies have incentive to keep people alive so that they remain as customers (end users).
The Profitable Diseases
What diseases are causing us to be ill? We can consider illness in terms of burden of disease. Disability-Adjusted Life Years (DALYS) can be used to measure the impact disease has on our lives. DALYs measure the total burden of disease. They include years of life lost due to premature death and years lived with a disability. One DALY equals one lost year of healthy life. Figure 18 breaks down burden of disease by disease type or injury.
Figure 18: Burden of Disease, World (2019)
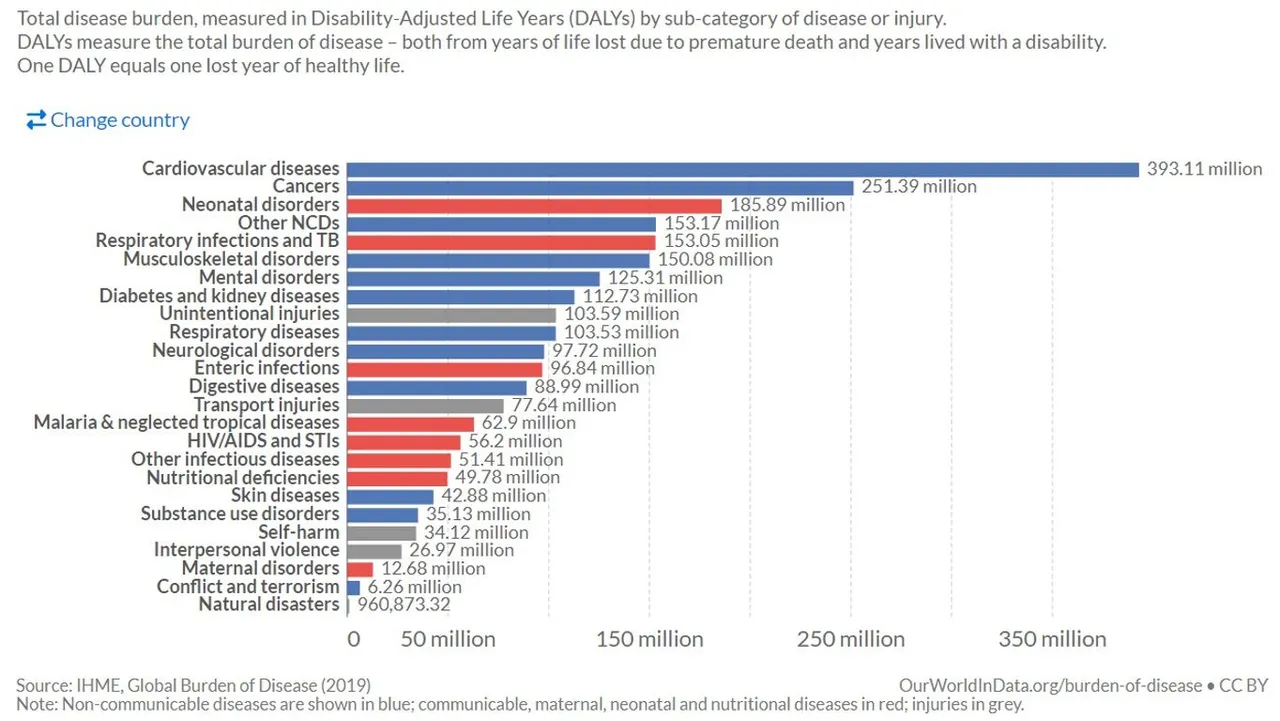
Source: Our World in Data
Cardiovascular disease is the biggest cause of illness and disability around the world followed by cancer, which is not a close second. People are mostly affected by non-communicable diseases but neo-natal disorders and respiratory infections are still quite high. Is the breakdown of disease different in developed countries? Data has been grouped based on income. Figure 19 breaks down burden of disease by disease type or injury for high income countries based on the World Banks definition.
Figure 19: Burden of Disease, High Income Countries (World Bank) (2019)
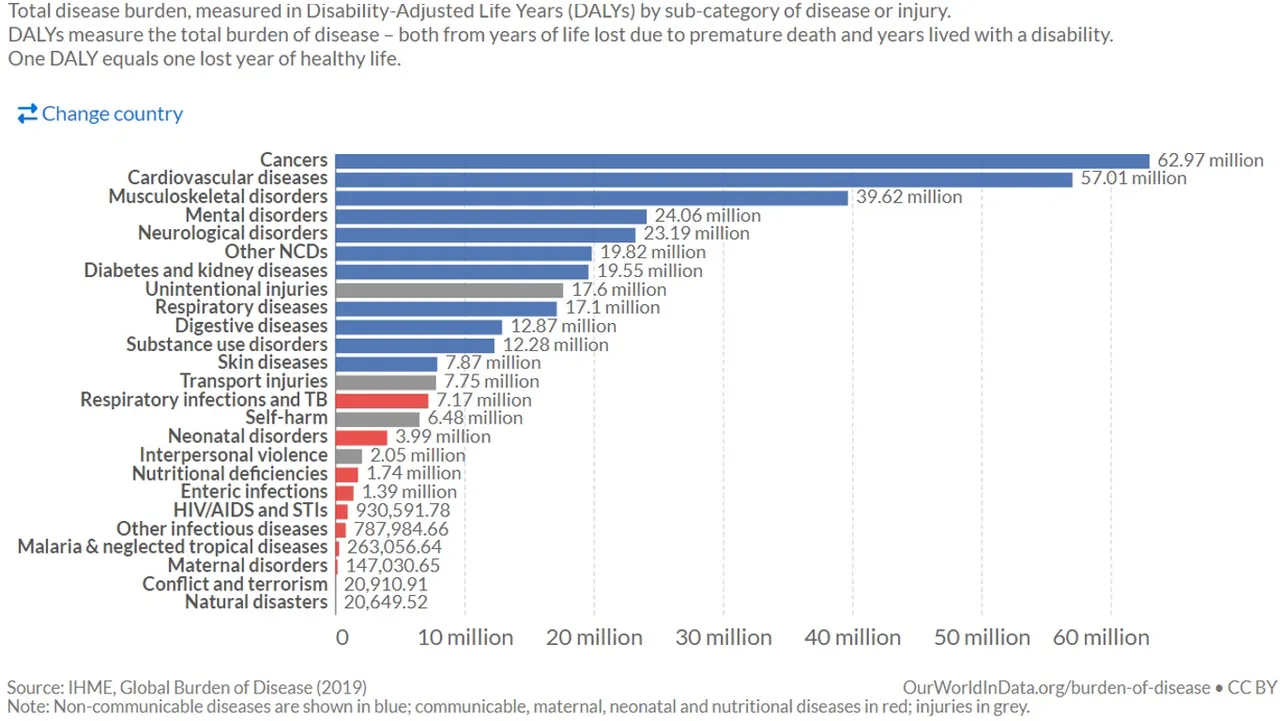
Source: Our World in Data
The breakdown of disease is different for the richest countries. Cancer has overtaken cardiovascular disease. The diseases with the highest burden of disease (DALYS) are all non-communicative. Respiratory infections and TB (most DALYs for a communicative disease) is not even ranked in the top 10. Why is there such a difference in breakdown? Wealthier countries have been more successful at combating communicative diseases than non-communicative diseases. Figure 20 compares non-communicative diseases with GDP per capita for a large sample of countries with vastly varying GDP per capita.
Figure 20: Burden of Disease of non-communicative disease vs. GDP per capita (2019)
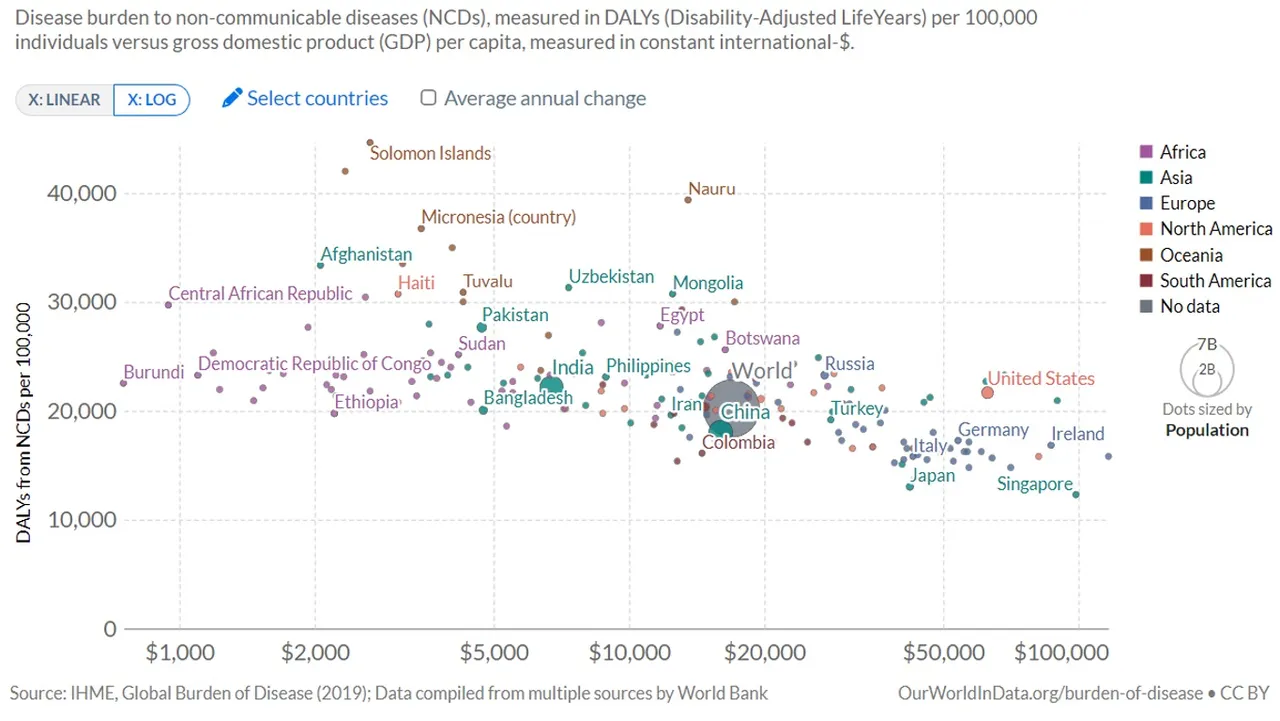
Source: Our World in Data
There appears to be minimal correlation between the prevalence of non-communicative diseases and per capita income. Therefore, we can argue that there is minimal correlation between non-communicative diseases and healthcare expenditure (see discussion earlier in post for relationship between income and healthcare expenditure).
Trends indicate that non-communicative diseases were decreasing at a decreasing rate per capita for high income countries until around 2014. After that, for a few years they remained constant and since 2017 have begun to increase. Figure 21 contains the breakdown of the burden of disease for non-communicative diseases for high income countries between 1990 and 2019.
Figure 21: Breakdown of non-communicative disease for High Income countries (World Bank (1990 to 2019)
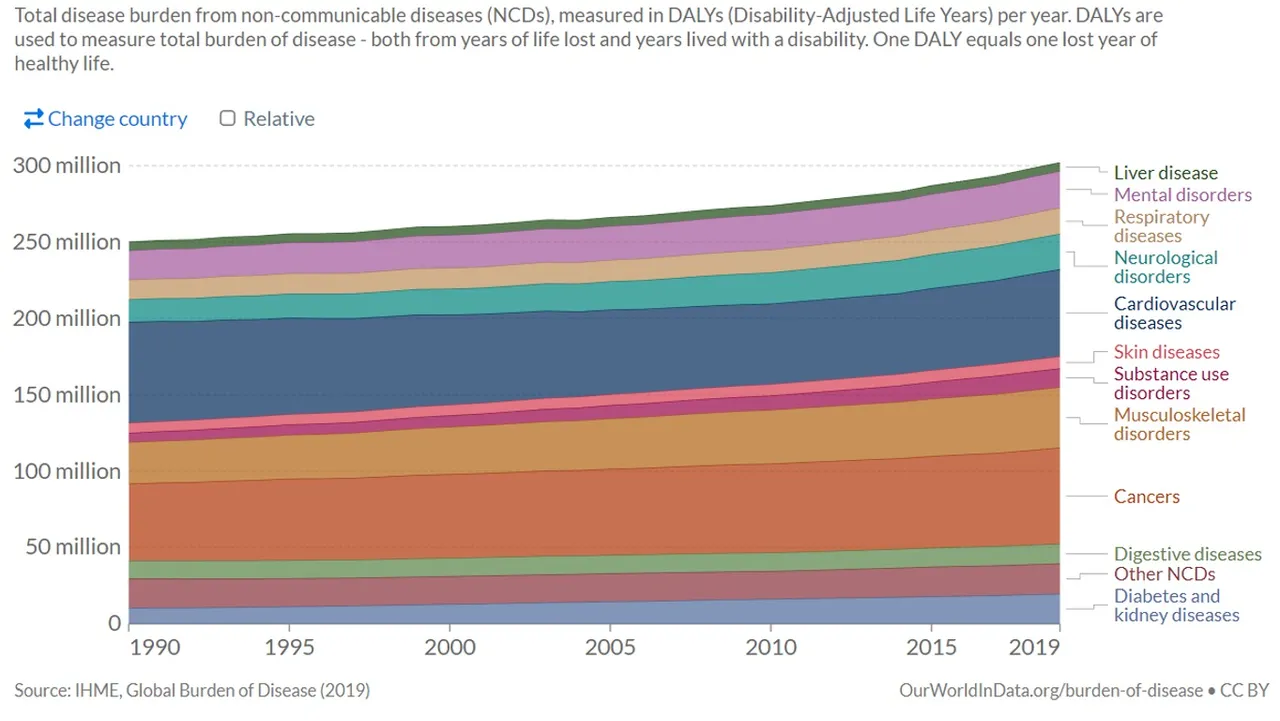
Source: Our World in Data
Non-communicative diseases have been increasing at a slightly increasing rate. Cardiovascular diseases have been declining for most of this period. Diabetes, and kidney disease, mental disorders, and musculoskeletal disorder, substance abuse, and cancers have been steadily increasing.
Cancers are one of biggest cause of disease around the world and highest cause of disease in high income countries. The impact of cancers are getting worse. Figure 22 contains data for the number of new cancer cases and the number of cancer deaths between 2002 and 2018 worldwide.
Figure 22: Trend in number of Cancer patients globally
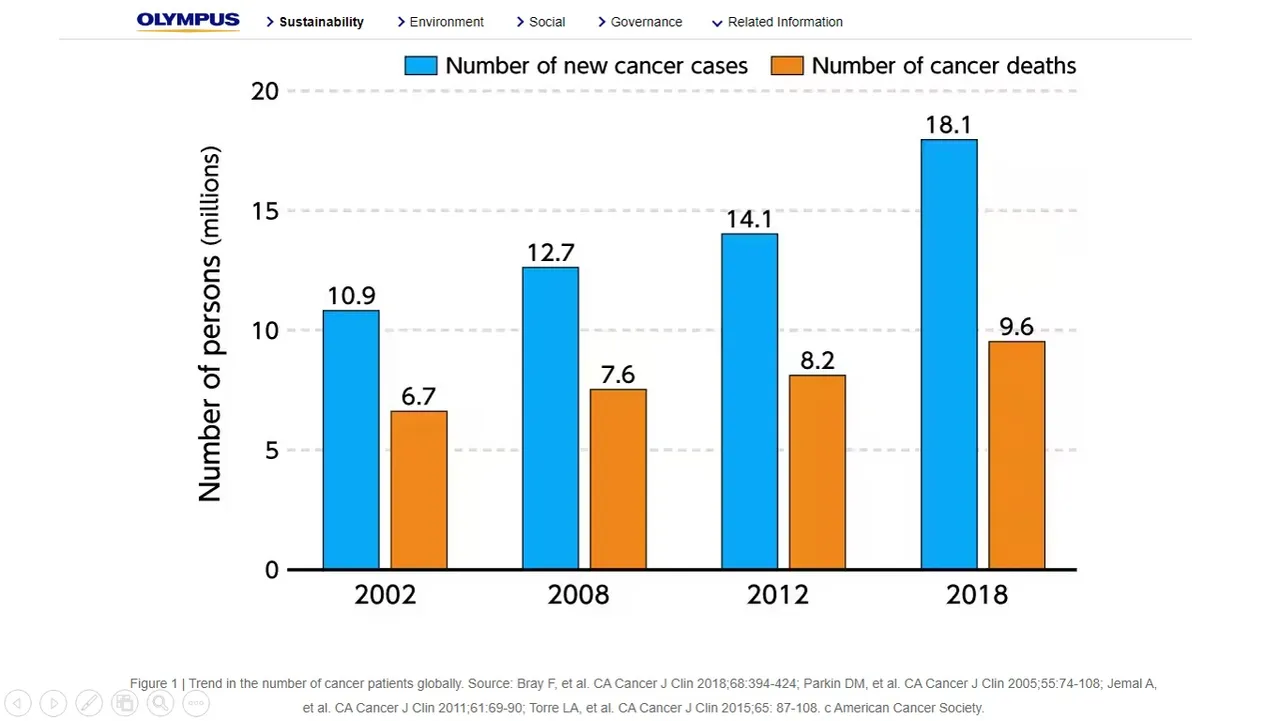
Source: Various sources cited by Olmpus
Cancer medications and treatments are very profitable for pharmaceutical companies. Revenue obtained from the sale of Cancer medication is by far the highest of any other medication in the world. Figure 23 compares worldwide revenue from various types of medication in 2018 as well as projected figures for 2024 based on the data available at the time the revenue figures for 2018 were published. Figure 24 contains more recent data for just cancer medication and treatments. It contains the revenue and market share for 2019 and projected revenue and market share for 2022 and 2025.
Figure 23: Prescription and over-the-counter medication revenue for 2018 and projected for 2024
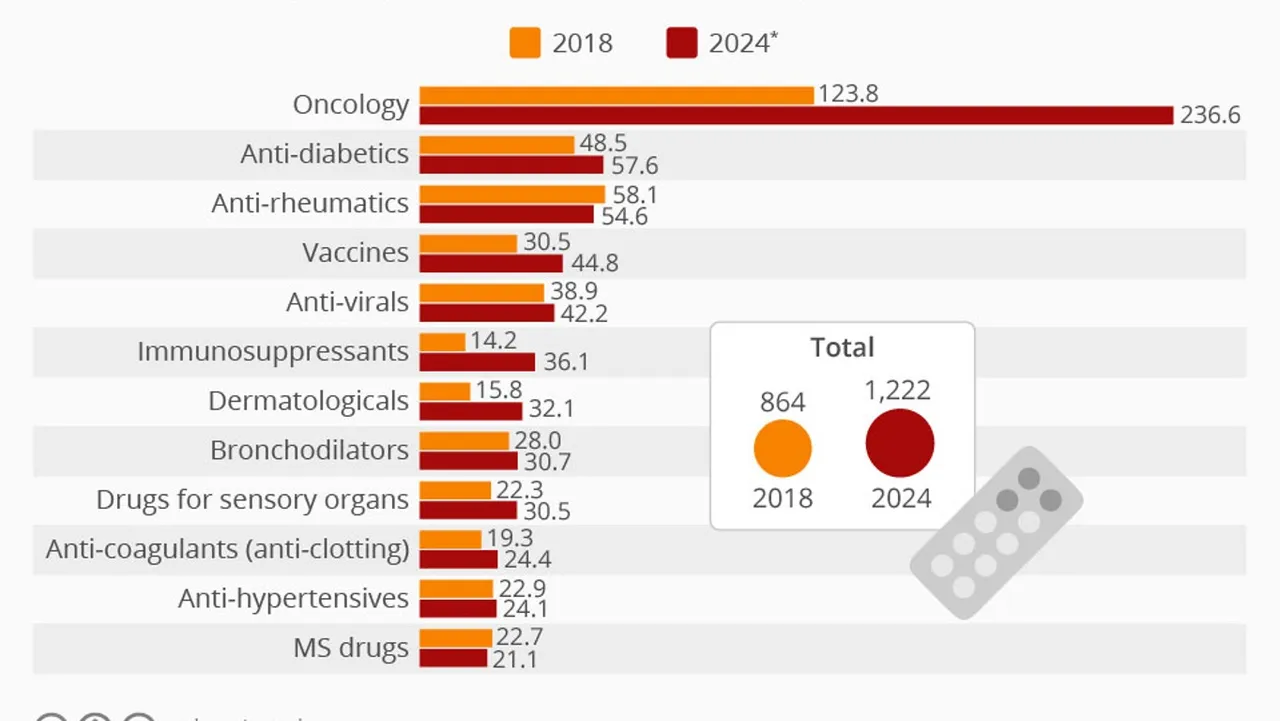
Source: Statista cited by My Republica
Figure 24: Revenue and market share of cancer medication and treatments
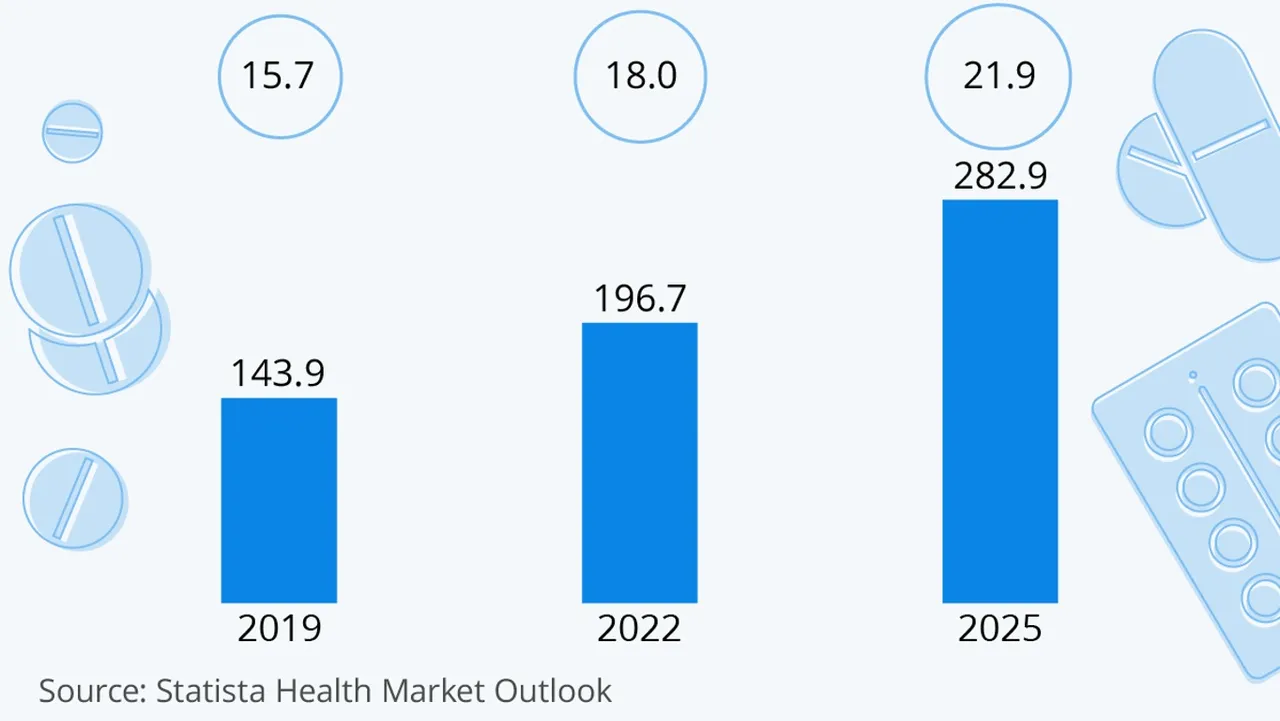
Source: Statista
The projections for the massive growth of cancer treatments and medications is also another indication that they are ineffective and are not expected to become any more effective in the near future.
The medication with the second and third highest revenue are anti-diabetics and anti-rheumatics. Diabetes and musculoskeletal disorders are two of the highest causes of disease and both are becoming more prevalent in high income countries (where the medicine is most easily available). Vaccines were fourth on the list (expected to climb after the Covid-19 fiasco). Vaccines are profitable because they are continued to be bought even if a disease is no longer prevalent. Vaccine advocates claim they remain necessary as a means to prevent the disease from becoming prevalent again. In my pre-Covid-19 post, A closer look at vaccines, I raise many questions about the usage of vaccines. Vaccine profitable is linked to targeting transmissible disease to reach more potential end users (I discuss my opinions regarding vaccines in more detail later in the post).
Cancer medication and treatment global markets are dominated by a small number of very large pharmaceutical companies. Figure 25 contains the revenue of the pharmaceutical companies that earnt the highest revenue for their cancer medication and treatments (oncology therapies) in 2017 and 2020.
Figure 25: Highest Oncology Therapy Revenues for 2017 and 2020
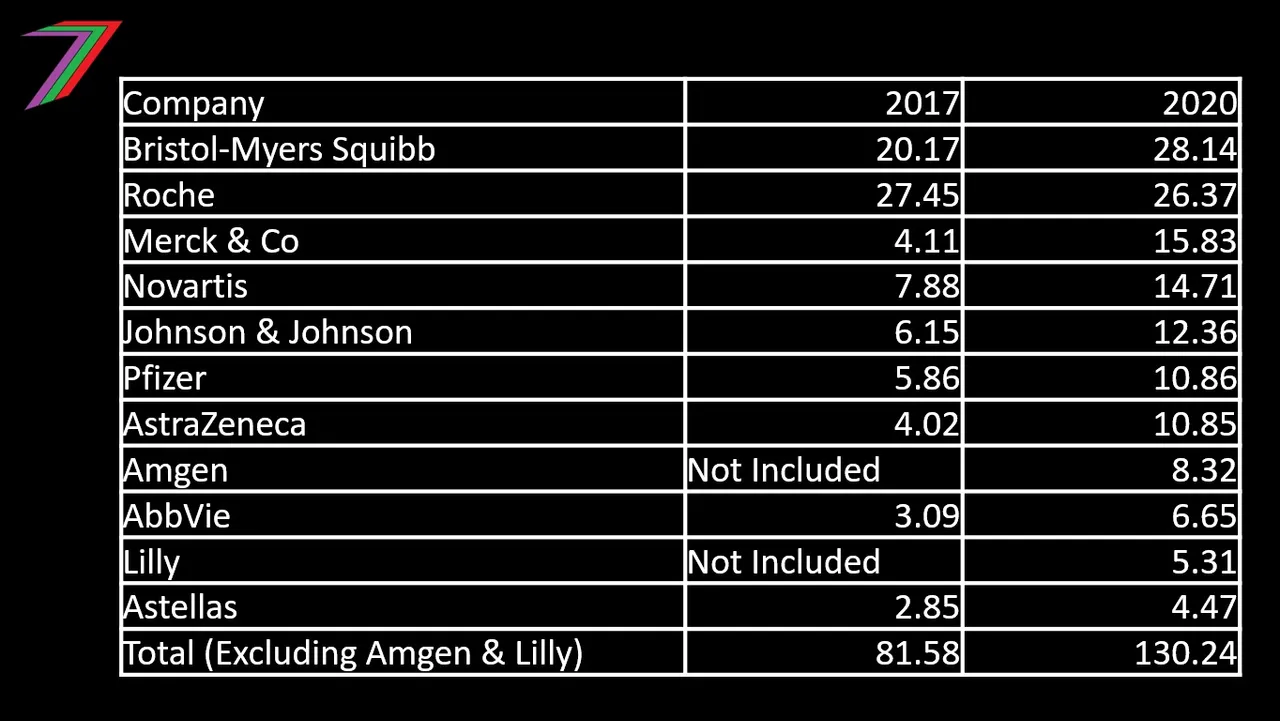
Sources: 2017 Data Fierce Pharma and 2020 Data Pharma Shots
Note: Bristol-Myers Squibb data for 2017 includes revenue for Celgene, which was acquired by Bristol-Myers Squibb in 2019.
For high income countries, cardio vascular disease has been mostly in decline over the past 30 years. However, the most recent data suggests that cardiovascular disease could be increasing. From 2014 to 2019, DALYS for cardiovascular diseases has been gradually increasing. The American College of Cardiology, identifies a global increase in cardiovascular related disease and deaths based on data available at the end of 2020. Since 2020, the situation appears to have become worse based on evidence linking heart disease to the Covid-19 jabs (see my post, Covid-19 Crimes and Vaccine Fraud).
It does not appear that pharmaceutical companies are able to profit as easily from cardiovascular disease as some of the other non-communicable diseases such as cancers. This might change soon. Pfizer have new heart medications Vyndaqel and Vyndamax. These medications generated over a billion US dollars in revenue for the year ending first quarter of 2021. This revenue may greatly increase in response to a spike in Covid-19 jab related heart conditions. Figure 26 contains the growth in revenue for these new medications.
Figure 26: Pfizer’s Vyndaquel/Vyndamax worldwide revenue
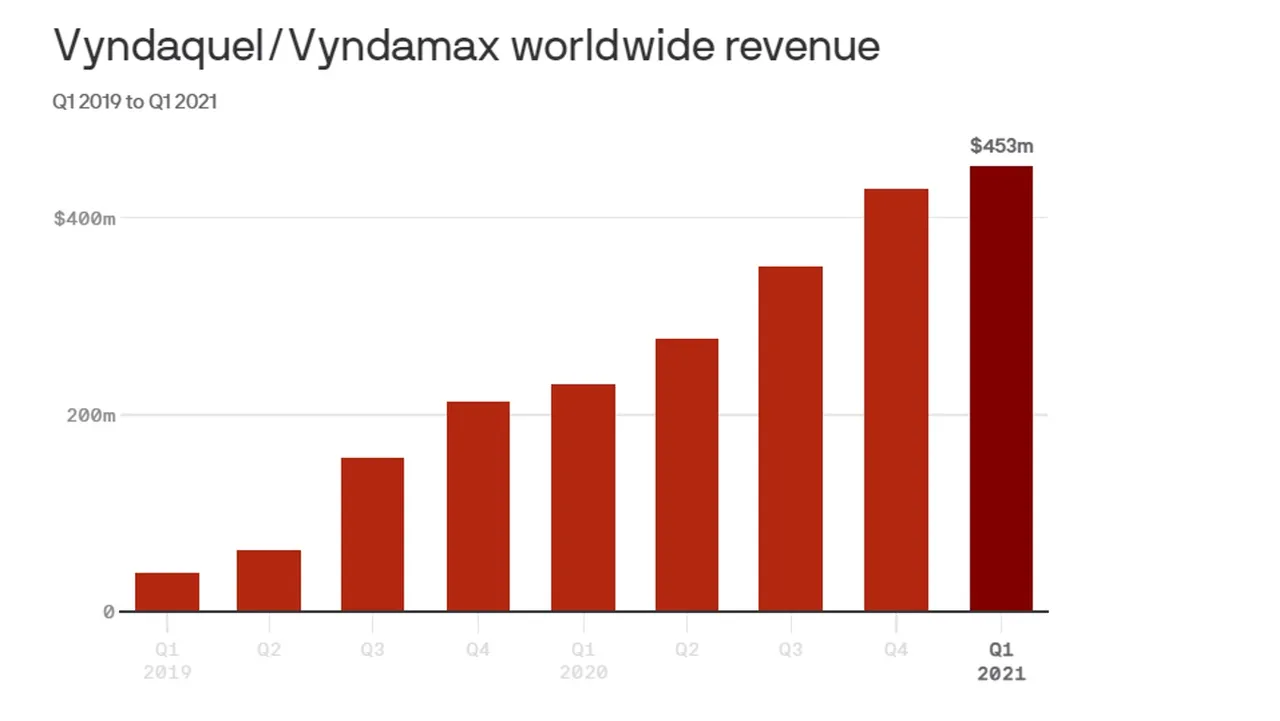
Source: Axios
Cancer medication and treatments have dominated pharmaceutical revenue and are projected to be a main source of revenue in the future. In 2021, Covid-19 temporarily boosted the sales of vaccines (by category not by function) for Pfizer with the Comirnaty jab (highest revenue in 2021) and Moderna with the Spikevax jab (third highest revenue in 2021). These jabs are marketed as vaccines. However, marketing by these companies was not necessary as Government health departments were the main customers for these jabs; Governments and mainstream media did all the marketing necessary for public uptake. Figure 27 contains the 2021 sales data.
Figure 27: Medication sales by medication and company
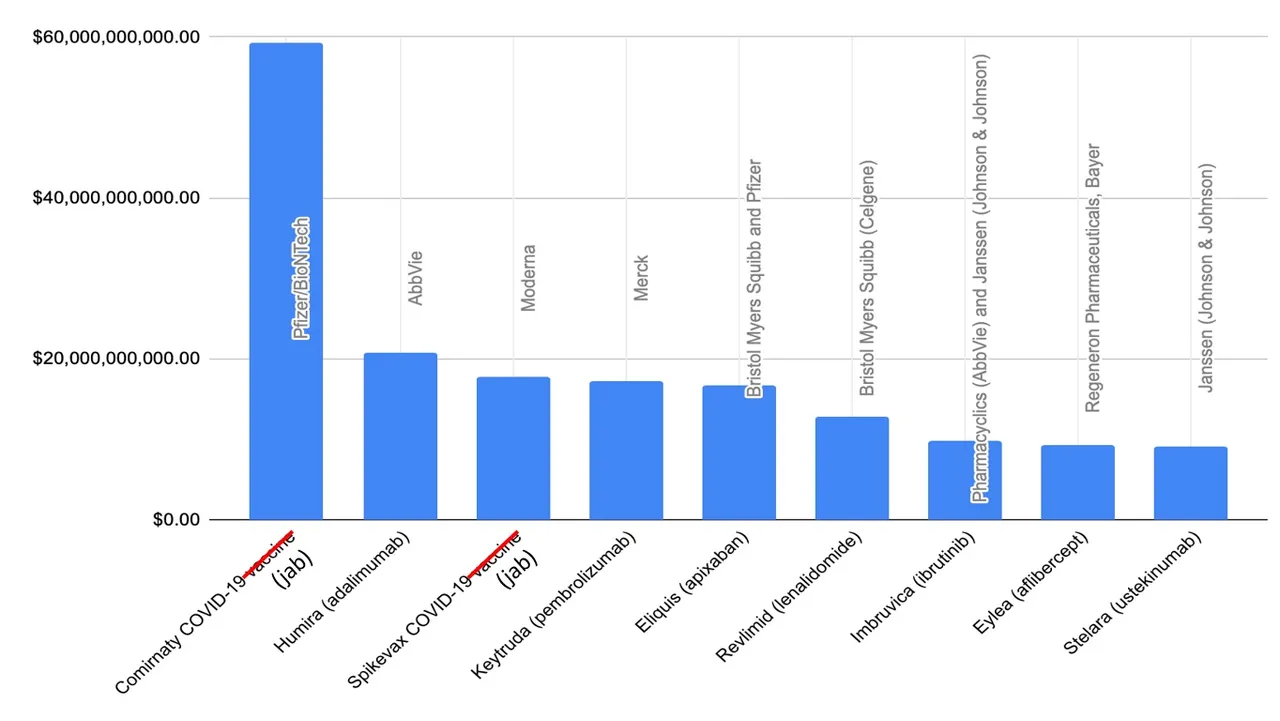
Source: Drug Discovery and Development
Notes:
| Medication Name | Treatment Type Summary |
|---|---|
| Comirnaty COVID-19 jab | Covid-19 |
| Humira (adalimumab) | rheumatoid and psoriatic arthritis |
| Spikevax COVID-19 jab | Covid-19 |
| Keytruda (pembrolizumab) | various cancers |
| Eliquis (apixaban) | blood clots |
| Revlimid (lenalidomide) | various cancers |
| Imbruvica (ibrutinib) | various cancers |
| Eylea (aflibercept) | age-related macular degeneration |
| Stelara (ustekinumab) | Crohn’s diseas |
My Opinions on Vaccines
Vaccination could be a good approach to preventing and protecting against virulent diseases that have a high mortality rate. However, in most cases, vaccines are unlikely to be viable solutions. Vaccines are difficult to develop and difficult to ethically test. For some diseases, vaccines might not ever be able to be developed. Vaccines can consume decades of research and testing and one might not ever be feasible for use; it might be ineffective and/or cause other disease or harm. The diseases most appropriate for prevention with a vaccine might not generate high revenue. According to hypothesises supported by evolutionary theory, there is a trade-off between virulence and transmission (i.e. the viruses that cause the most harmful disease do not spread quickly) (Francois Blanquart et al). This is likely to reduce the market for a vaccine for a disease that can be more easily contained. Many diseases become less virulent as they mutate. If a vaccine is successfully developed, it might have a low demand as the disease it was designed to prevent can be cured or managed with existing treatments. It is also possible that the vaccine is less effective against the prevailing variant or future variants.
If the intention was to minimise the harm caused by Covid-19, attempting to develop a vaccine was an absurd first response. Covid-19, even when it was claimed to have been identified, was not life threatening to the vast majority of the population. Data suggests that only elderly people with serious pre-existing conditions were highly vulnerable to the disease (Off Guardian, Robert Verity et al 2020, and other various research). There were alternative existing medication that could further reduce the chances of serious illness (e.g. Vitamin D, Hydroxychloroquine, zinc, and Ivermectin). SARS-CoV-2 (Covid-19 virus) was reported to mutate quickly and in some cases significantly; thus, reducing the effectiveness of any vaccine. By the time an effective and safe vaccine could be made available to the public, possibly a decade later, it would not be necessary as Covid-19 would be manageable or even non-existent. The Middle East Respiratory Syndrome (MERS-CoV) would have been a better candidate for vaccine development. In my post, Outline of a possible Cost Benefit Analysis Framework for Covid-19 Vaccines, I discussed how a Cost Benefit Analysis for a Covid-19 vaccine could have been conducted.
The Covid-19 jabs were not vaccines (see my post, Covid-19 Crimes and Vaccine Fraud for a detailed explanation regarding the Covid-19 jabs). They escaped scrutiny because they had a limited number of customers; mostly Government. Governments choose not to scrutinise the products they purchased or did not care that they were going to destroy the lives of thousands or possibly millions of people they were supposed to be representing. Governments even protected these companies from legal action. The relationships between Government, pharmaceutical companies, and any other major parties that stood to benefit from the mass distribution of these jabs was more important than the people receiving the jabs. If the people were the direct customers of the jabs (i.e. were required to purchase the jabs with direct payments), the pharmaceutical companies would not have attempted to develop them as their expected revenue would not have been secured.
Healthcare for Who?
Expenditure on healthcare is high. It is increasing in terms of percentage of GDP around the world (see Figures 12 and 13). Most of this expenditure is not determined by the people of these countries. Instead, it is determined by Governments and pharmaceutical companies who have considerable monopoly power on a global scale. Figure 28 compares mandatory Government expenditure on healthcare with voluntary expenditure made by people.
Figure 28: Healthcare Expenditure Government (Mandatory) vs. Voluntary (2019)

Source: OECD Data
For the countries that spend the most on healthcare, Government mandatory expenditure far exceeds voluntary expenditure made by people (more than 5 times more for many countries). Governments are the customers for healthcare products. The people are required to accept the decisions the Government make on their behalf.
Pharmaceutical companies may have as much power over healthcare expenditure as Governments. Pharmaceutical companies are part of a global oligopoly market structure (see post, Oligopoly – The market structure that does not let the market decide for an explanation on how oligopolies operate in many different markets) that gives them considerable monopoly power. Figure 29 contains the market cap of the 20 largest pharmaceutical companies in world. Most of these companies have markets in many countries in the world.
Figure 29: Market Cap of the 20 largest pharmaceutical companies in the world (2022)
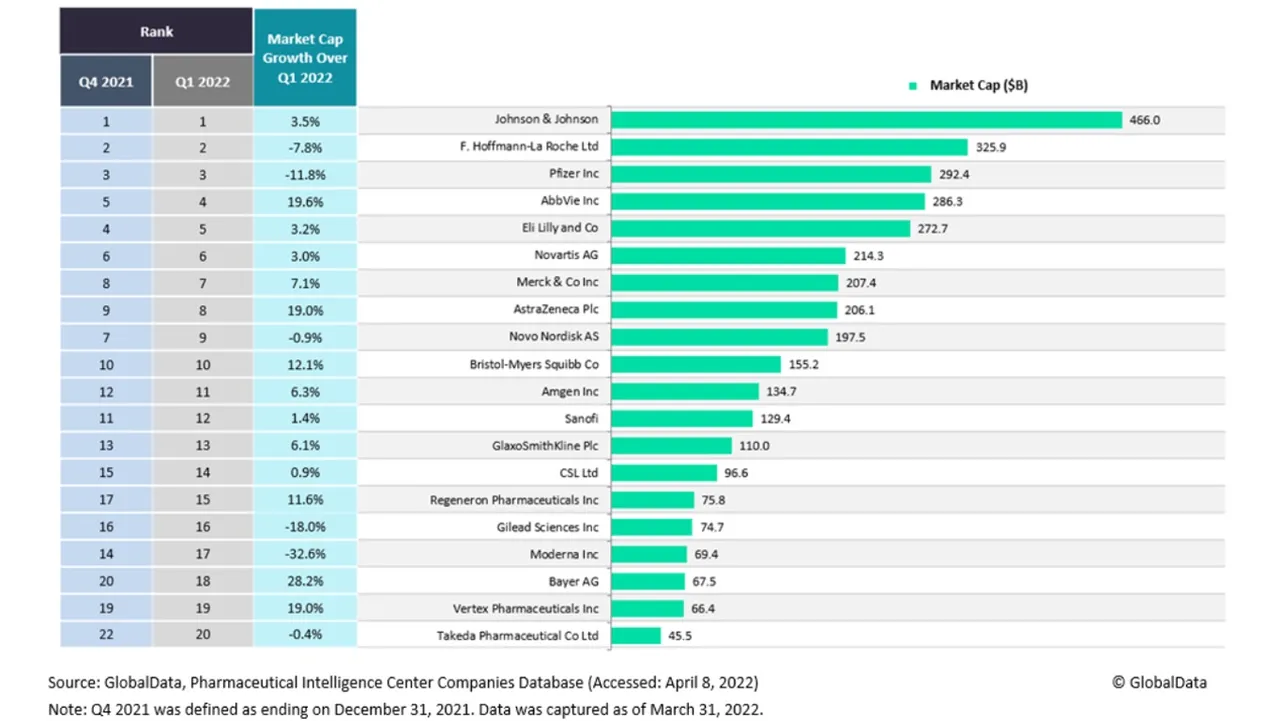
Source: Pharmaceutical Technology
Of the top 20 largest pharmaceutical companies in the world, the five largest companies have equivalent to almost 50% of that total market cap. Outside the largest 20, the market caps of pharmaceutical companies are small (e.g. 20th ranked company has less than 10% the market cap of the largest company). A few companies have considerable influence on what medicine is researched, developed, and sold. This arrangement is very profitable for them. Figure 30 contains the 2022 revenue for the world’s largest pharmaceutical companies. Revenue is broken down into pharmaceuticals, medical devices/diagnostics, and consumer health/nutrition/aesthetics.
Figure 30: Pharmaceutical companies’ revenue (2022)
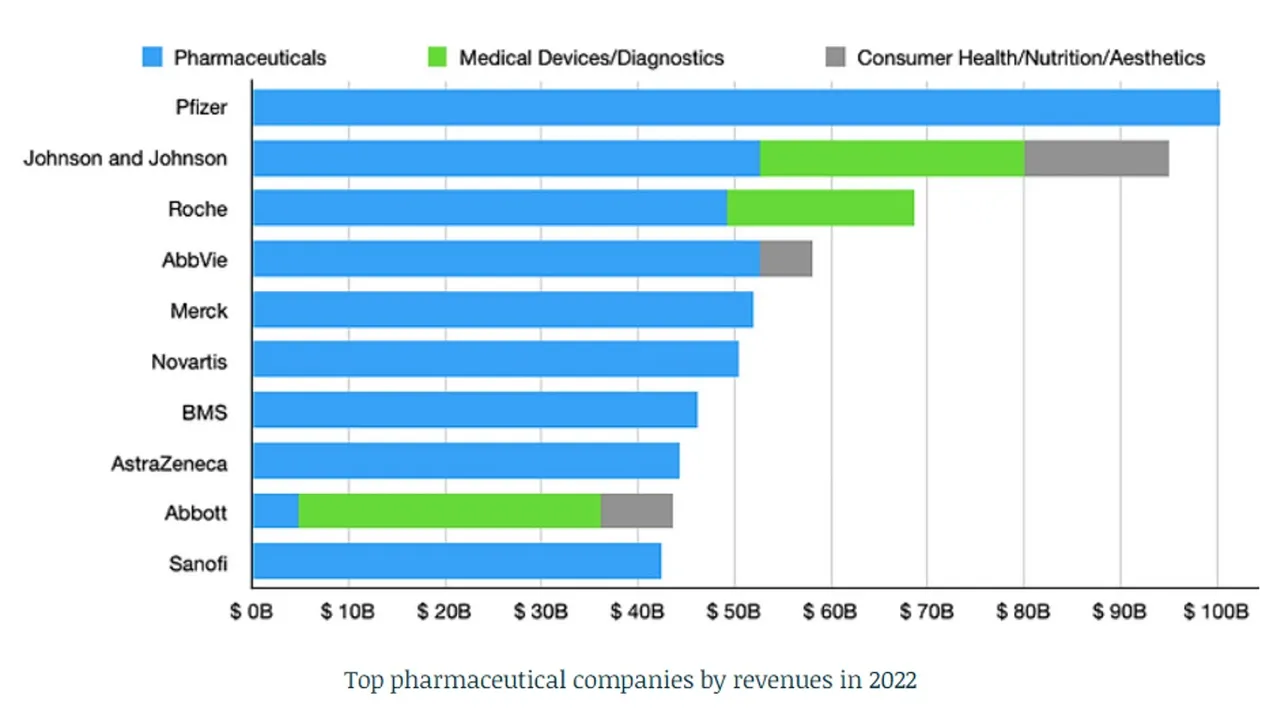
Source: iPharma Center
This revenue is trending upwards as we can see in Figure 31, which contains US pharmaceutical revenue from 2010 to 2020.
Figure 31: Us Pharmaceutical Industry Revenue (2010 to 2020)
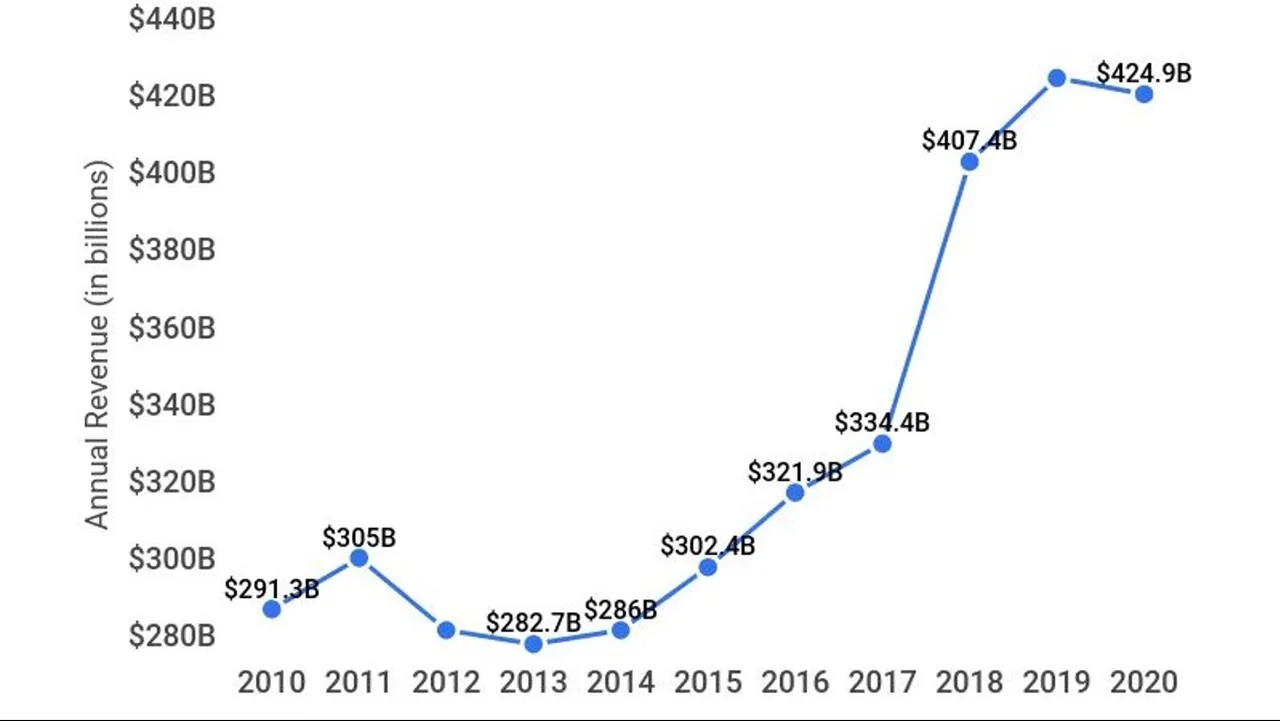
Source: Zippia
Pharmaceutical companies’ relationship with Governments means that they do not need to address the needs of the people using their products. They only need to have an arrangement with Government officials and representatives. The Governments take the role of convincing people that their expenditure on healthcare is good. They also claim that healthcare is free because the Government pay the costs and people can use healthcare facilities and products when deemed needed without needing to pay at the time of consumption. They fail to mention that Government money is the people’s money. The healthcare is not free, payment is either prepaid or deferred.
The misconception of ‘free’ leads to a form of moral hazard and wasted usage of resources. People become less careful with their own health because they have a safeguard (“free” healthcare). People are also likely to overuse the healthcare that is offered because they do not have to pay to use. Doctors are also more likely to overprescribe medication because it does not affect their costs. People will become less likely to pay for more appropriate healthcare that is not covered by the Government even though it might cost less.
Pharmaceutical companies do not only have close relationships with Governments. They have close relationships with media and the entertainment industry. Mainstream media promote the types of therapies offered by pharmaceutical companies even if they do not mention them by name or company, which is not necessary considering there are very few dominant pharmaceutical companies. Celebrities and actors also promote their products. This could be directly through paid advertisements or more effectively as a matter of their own proclaimed opinion. The biggest pharmaceutical companies sponsor television and movie award events as a way of securing their relationship (Endpoints News).
People want good health and not healthcare
Health is a complicated matter. People’s health can vary for many different reasons. This includes genetics, lifestyle, and misfortune. I believe that good health is a universal desire. Good healthcare is just a possible means for reaching the desired goal of good health (referred to as derived demand in economics).
The current healthcare systems treat healthcare as the desired product and the desired outcome. The relationship between Governments and pharmaceutical companies prevent the people from determining the product they want and do not fully enable the pursuit of the desired outcome, which is good health (not healthcare). Free markets are not allowed to operate. If they were allowed to operate, the response to health would be very different and I believe would be vastly improved. Free markets alone are not the full solution and will not enable everyone to obtain and maintain good health. Therefore, the community will need to provide support. This help could come in the form of contributing and distributing financial support to people who are unable to fund the required responses to address their health problems.
Free Markets
Since a free market response to health is currently barely existent, we can only hypothesize what it might resemble. Therefore, I will describe a possible free market response that would be able to achieve desired health outcomes. I believe we would have two main markets. One market for maintaining good health and the prevention of disease and one market for cures. A market for treatments will still exist but would become less lucrative based on a focus on good health.
The prevention market would be focused around obtaining and maintaining a healthy lifestyle and living. It would focus on what we put into our bodies as well what we do with our bodies. To meet this market, healthcare professionals would become better versed on how our actions affect our health. They would be able to provide better advice that would enable people to live a fulfilling life while minimising the risk to their own health. I would expect healthcare professionals in this market to introduce healthy living concepts to people at a young age. They would be guest speakers at schools, colleges and other learning institutes. Some may even become full-time staff members.
The cures market would be focused on returning us to good health rather than treatment. Therefore, people would be paying for good health and not a particular treatment or even a cure. If the response provided by healthcare professionals does not result in us returning to good health, we do not pay for the response provided. Demand for cures would be higher as they would be used to return us to good health without continued intervention. Demand for treatment would be minimal as they do not restore our health without creating dependency. Profits from treatments would fall as revenue would be based on the outcome of restored health instead of output of a medical product, which earns revenue from each purchase made.
Free markets will create competition between healthcare providers. A person might not be happy with the recommendations or pricing of a particular healthcare consultant. Therefore, they might choose another one who offers them closer to what they want. Initial consultations could be done in person or online. This could depend on the nature of the symptoms. Healthcare providers will need to offer people what they want or they will go out of business. Free markets also creates opportunities for cooperation between healthcare providers. This can enable them to operate joint programs and therapies that might be too expensive to do on an individual basis.
Community controlled Health Fund
Free markets cannot adequately provide for everyone. Some people have poor health through no fault of their own and some people have limited funds; therefore, might not be able to afford to pay for the recommended path that will return them to good health. Healthcare professionals can assess people’s medical conditions to determine if they need financial assistance to support obtaining better health or at least preventing any further deterioration of health. The aim should be to help people reach a level of health that can enable them to have a reasonable quality of life. A possible solution is a health fund. The fund could be financed through donations and through increased money supply (similar to how new coins are created for cryptocurrencies). The rules for distributing resources from this fund should be determined by the community; it would operate like a decentralised autonomous organisation (DAO). The methods of distribution will vary between communities.
Those running the health fund would still be met with various challenges. Decisions become even more difficult when operating on a tight budget. For example, how should the fund respond to people with self-inflicted illness, disease, and injury? Would society be tolerant of people using resources when they should not need them? Their usage could come at the expense of people who did not inflict harm upon themselves. In some cases, this could be difficult to determine. In other cases, mental disorders could have played a role in the self-infliction. This adds to the complexity of funding healthcare through a fund. However, solutions can be reached through consensus. There is a desire to reach good outcomes as they also affect the people involved in the decision-making process.
Final Thoughts
Our current health systems do not work for the people and they appear to be getting worse. We need to move away from dependence on Government and very large pharmaceutical companies. We need a free market approach that enables people to obtain or remain in good health. Good health is the desired outcome and not healthcare. Competition for meeting the goal of good health will help bring the costs and prices of health provision to a manageable level that should be affordable under most circumstances. These costs would become payable once a person has returned to good health. Under circumstances where health problems require unaffordable responses, there should be community controlled resources available to support people who need these expensive responses.
The biggest problem we face in improving health and healthcare systems is the transition away from the entrenched system. Governments will not willingly concede power. Very large pharmaceutical companies will not let their very large market share go. They have too much to lose from actual solutions to improving health. For example, a cure for cancer would take away a huge chunk of their revenue. I would expect them to go to great extent to prevent that cure ever reaching the wider public. I imagine they probably have already done so.
How will change actually occur? It could happen gradually through people opting out of Government run health systems. I believe many people have switched to more traditional medicine and adopted healthier lifestyles. The rate of this type of change is slow and may never become the standard way of approaching health for most people. It could happen more rapidly as Governments, countries, and economies completely collapse. The biggest risk with rapid change is that the rapid solution put in place is no better or even worse than one originally in place.
More posts

If you want to read any of my other posts, you can click on the links below. These links will lead you to posts containing my collection of works. These 'Collection of Works' posts have been updated to contain links to the Hive versions of my posts.
Hive: Future of Social Media

Spectrumecons on the Hive blockchain