I felt a great disturbance in the Force. As if millions of voices suddenly cried out in terror and were suddenly silenced.”
— Obi-Wan Kenobi
INTRODUCTION
Maybe you're tired of hearing the word malaria, but an image of the quote above flashes in my mind when I think of deaths from a ravaging disease like malaria. It's rather unfortunate that you won't stop hearing about it soon until we do to it what's been done to polio. In the Tropics, malaria is a household name, not on the positive side though. It has earned for itself a title the "everyday sickness" because every day, I get to dispense malaria medications, more than any other drug. There is hardly anyone in Nigeria who has not been treated for malaria in his/her lifetime.
Malaria ranks among the major health challenges of the world, and despite great international efforts, malaria still inflicts an enormous toll on human lives, especially in Africa. I think of the war against malaria as a full-scale global war.

Malaria, an ancient and enduring scourge, has been around for about 4000 years and has significantly influenced the human population (it actually threatened that of the Roman Empire). According to the WHO, there were 216 million cases of malaria in 91 countries; 5 million more than what was reported in 2015, claiming about 445,000 lives. The scourge claims the life of a child every 2 minutes and children under the age of 5 are more susceptible. 80% of the global malaria burden is carried by 15 African countries (most of which are in Sub-Saharan Africa), while worldwide, the African region suffers 90% of malaria cases and 91% of malaria-related deaths worldwide. Nigeria accounts for 27% of malaria cases and 24% of malaria-related deaths globally. source
The malaria parasite has been killing children and sapping the strength of whole populations for tens of thousands of years. It is impossible to calculate the harm malaria has done to the world.
_Bill Gates
Malaria from the Italian mal aria which literally translates to “bad air” is caused by a protozoan parasite known as Plasmodium. 6 species of Plasmodium are known to cause malaria in humans (P. ovale actually have to subspecies). They include:
- P. falciparum: this species is known to cause about 50% of malaria cases, and it is the deadliest of all forms of malaria. It is actually considered the deadliest parasite in humans.

- P. vivax: this form is the most frequent cause of recurring malaria. It is less virulent than P. falciparum but can lead to death due to splenomegaly (abnormal enlargement of the spleen). It also has the ability to lie dormant in the liver (in a form known as hypnozoite) from where it periodically reactivates to cause relapses of P. vivax malaria. Hence, a single P. vivax infection can give rise to multiple episodes of malaria, in the absence of a new mosquito bite. These relapses can occur weeks, months or even years after the initial infection.
- P. malariae: this form is known to cause what is known as “benign malaria” as it not as dangerous as falciparum or vivax malaria.
- P. ovale: this form is rare compared to P. falciparum and P.vivax and to a very large extent less dangerous than P. falciparum. It has 2 subspecies known as P. ovale curtisi and P. ovale wallikeri.
- P. knowlesi: these lesser-known species cause malaria in macaque monkeys but it may also affect humans. It accounts for 70% of malaria cases in certain areas of Southeast Asia where it is prevalent.
THE WAR FOR SURVIVAL
In order for man to win the war against this deadly parasite, man had to develop a strategy and gather all information that they could about the parasite. One major breakthrough was knowing the life-cycle of the parasite. The natural ecology of malaria parasite involves the parasite infecting successively two hosts: humans and female Anopheles mosquitoes.
The disease is transmitted through the bite of an infected female Anopheles mosquito. An Anopheles mosquito gets infected (but not sick) from a previous blood meal on an infected person. The parasites picked up from this individual multiplies in the mosquito's salivary gland. When the mosquito takes its next blood meal (usually around 10 days), the mosquito bites an uninfected person and introduces the microscopic parasites from the mosquito’s saliva into a person’s blood.
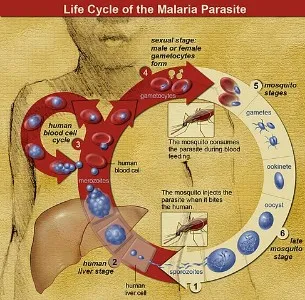
In humans, the parasites travel to the liver where they mature and reproduce first in the liver cells and then in the red cells of the blood. In the blood, successive broods of parasites grow inside the red cells and destroy them, releasing daughter parasites (merozoites) that continue the cycle by invading other red cells.
The blood stage parasites are those that cause the symptoms of malaria. When certain forms of blood stage parasites (gametocytes) are picked up by a female Anopheles mosquito during a blood meal, they start another, different cycle of growth and multiplication in the mosquito. After 10-18 days, the parasites are formed (as sporozoites) in the mosquito’s salivary glands. When the Anopheles mosquito takes a blood meal on another human, the sporozoites are injected with the mosquito’s saliva and start another human infection when they parasitize the liver cells. Thus, the mosquito carries the disease from one human to another (acting as a “vector”). Differently, from the human host, the mosquito vector does not suffer from the presence of the parasites source.
Following an infective bite of a female Anopheles mosquito, it could take from 7 days to 4 weeks incubation period for the symptoms to manifest. Malaria by P.ovale and P.vivax can occur again (relapsing malaria) after treatment as some of the parasites can remain dormant in the liver for many months up to 4 years.source Infection with malaria parasites may result in a wide variety of symptoms ranging from absent or very mild symptoms to severe disease and even death.
Malaria disease can be categorized as uncomplicated or severe (complicated). In general, malaria is a curable disease if diagnosed and treated promptly and correctly. All the clinical symptoms associated with malaria are caused by the asexual erythrocytic or blood stage parasites. When the parasite develops in the erythrocyte, numerous waste substances such as hemozoin pigment and other toxic factors accumulate in the infected red blood cells. These are dumped into the bloodstream when the infected cells lyse and release invasive merozoites. The hemozoin and other toxic factors such as glucose phosphate isomerase (GPI) stimulate macrophages and other cells to produce fever and rigours and probably influence other severe pathophysiology associated with malaria.source
Common signs and symptoms associated with uncomplicated malaria include:
- Fever.
- Chills.
- Sweats.
- Headaches.
- Nausea and vomiting.
- Body and joint aches.
- General malaise.
- Enlarged spleen.
- Mild jaundice.
- Enlargement of the liver.
- Increased respiratory rate.
Plasmodium falciparum-infected erythrocytes, particularly those with mature trophozoites, adhere to vascular endothelium of venular blood vessel wall and do not freely circulate into the blood.
When this sequestration of infected erythrocytes occurs in the vessel of the brain, it is believed to be a factor in causing the severe (malaria) disease syndrome associated with high mortality.source Eventually, the infection is complicated by serious organ failures and/or abnormalities in the patient’s blood or metabolism. Severe malaria occurs most often in individuals with little or no immunity to malaria. This group include all residents of areas with low or no malaria transmission, and young children and pregnant women in areas with high transmission.
Signs and symptoms associated with severe malaria include:

- Cerebral malaria, with abnormal behaviour, impairment of consciousness, seizures, coma, or other neurologic abnormalities
- Severe anaemia due to hemolysis (destruction of the red blood cells)
- Hemoglobinuria (haemoglobin in the urine) due to hemolysis
- Pulmonary oedema (fluid buildup in the lungs) or acute respiratory distress syndrome (ARDS), which may occur even after the parasite counts have decreased in response to treatment
- Abnormalities in blood coagulation and thrombocytopenia (decrease in blood platelets)
- Cardiovascular collapse and shock
- Acute kidney failure
- Hyperparasitemia, where more than 5% of the red blood cells are infected by malaria parasites
- Metabolic acidosis (excessive acidity in the blood and tissue fluids), often in association with hypoglycemia
- Hypoglycemia (low blood glucose). Hypoglycaemia may also occur in pregnant women with uncomplicated malaria, or after treatment with quinine.source
THE WEAPONS OF OUR WARFARE
Asides the use of Insecticide-treated mosquito nets (ITNs), insecticides and hygienic environmental practices to combat malaria, antimalarial drugs has been the most powerful weapon used in the fight against malaria. Drugs used in the treatment of malaria depends on the form of the malaria parasite and the severity of the disease. Simple or uncomplicated malaria are treated with oral medications, while severe or complicated malaria is a medical emergency and treatment involves supportive measures that are best done in the critical (intensive) care unit.source Examples of drugs developed for the treatment of malaria over the years include:
- Cinchona alkaloids (e.g. Quinine, Quinidine);
- 8-aminoquinoline (e.g. Primaquine, Tafenoquine, pamaquine);
- 4-aminoquinoline (e.g. Chloroquine, Hydroxychloroquine, Amodiaquine);
- Quinoline methanol (e.g. Mefloquine)
- 9-aminoacridine (e.g. Mepacrine);
- Biguanide (e.g. Proguanil, Chlorproguanil);
- Diaminopyrimidines (e.g. Pyrimethamine, Trimethoprim);
- Sulfone and Sulfonamides (e.g. Sulfadoxine, Dapsone);
- Phenanthrene-methanols (e.g. Halofantrine, Lumefantrine);
- Naphthoquinones (e.g. Atovaquone)
- Antibiotics (Doxycycline, Clindamycin) and others source.
Despite the numerous drugs developed to win this war, upgrades and updates of older drugs emerged and they themselves eventually became outdated. The usefulness of these antimalarial agents are, however, compromised by two major factors; the relatively not too many anti-malarial drugs currently licensed for use or those proceeding to large-scale clinical trials and the inevitable emergence and spread of parasite strains that are resistant to the conventional drugs that have been licenced.
Such resistance can rise rapidly from a combination of circumstances that, in the host population, include overuse of drugs for prevention (prophylaxis), and incomplete therapeutic treatments of infected patients, either by lack of compliance or the unsuspecting use of counterfeit drugs deficient in the recommended dose, and in the parasite population, include genetic and metabolic flexibility together with a vast rate of reproduction and dispersal of resistance genes (crt, mdrl, dhfr/dhps and others) via asexual recombination in the mosquito.source The emergence of resistance took several decades for quinine, 12 years for chloroquine, 5 years for mefloquine and approximately 1 year for proguanil, sulfadoxine-pyrimethamine and atovaquone.source Following this incidence, the WHO has since 2001, recommended the use of artemisinin-based combination therapies (ACTs) for treating falciparum malaria where resistance to monotherapies or non-artemisinin combination therapies (e.g. sulfadoxine-pyrimethamine) is prevalent source.
There was a need for structurally unconventional antimalarials active against resistant strains of P. falciparum and this brought about the discovery of artemisinin and its derivatives, a unique sesquiterpene lactone isolated from Artemisia annua. The artemisinins are known for their potent antimalarial activity as they show very rapid parasite clearance and faster resolution of symptoms than any other currently licenced antimalarial drug.source The parent compound of this class is artemisinin, where dihydroartemisinin, artesunate, artemether, and β-arteether are the most common derivatives of artemisinin. They are more effective in the treatment of P. falciparum infection when used in combination with other antimalarials (known as artemisinin-combination therapy, or ACT), which decreases resistance to any single drug component. These additional antimalarials include amodiaquine, lumefantrine, mefloquine or sulfadoxine/pyrimethamine. Another recommended combination is dihydroartemisinin and piperaquine. ACTs are about 90% effective when used to treat uncomplicated malaria.source
The artemisinins, however, aren’t the ideal antimalarial drugs. For instance, the short half-life of the drug is attributed to poor cure rates and a high rate of recrudescence (>25%) for short courses (3-5 days) of treatmentsource. Also, the artemisinins, are, unfortunately, yielding to the power of resistant strains. There are reports of strains found in individuals living in the Cambodia-Thailand border which are resistant to combination therapies that include the artemisinins.source If nothing is done urgently, it's only a matter of time for these strains to find their way into other regions and malaria may become untreatable. Resistance in these areas isn’t unconnected to regimens involving monotherapy at sub-therapeutic doses and substandard products of artemisinin and their combinations flooding the market.
A NEW HOPE
“Help me, Obi-Wan Kenobi. You’re my only hope.” — Leia Organa
“Help us Tafenoquine. You’re our new hope.” _FDA
The United States Food and Drug Administration (FDA) actually didn’t say that to tafenoquine but probably meant it by recently approving the use of Krintafel® (tafenoquine) for the radical cure of P. vivax as part of its contribution towards malaria eradication efforts. The dormant liver forms of the parasite cannot be readily treated with most anti-malarial treatments active against the blood-stage parasite. Before now, the 8-aminoquinoline, primaquine, was the only FDA approved medicine that targets the dormant liver stage to prevent relapse. It must be taken for 14 days to be effective, a regimen that is associated with poor compliance.source The main advantage of tafenoquine is that it has a long half-life (2–3 weeks) and therefore a single treatment may be sufficient to clear hypnozoites. The shorter regimen has been described as an advantage.

Tafenoquine belongs to the 8-aminoquinoline class of antimalarial drugs. It is a 5-phenoxyl derivative of primaquine jointly developed by the Walter Reed Army Institute of Research (WRAIR) and GlaxoSmithKline Pharmaceuticals for the treatment and prevention of relapsing P. vivax malaria in patients 16 years and older.source
MECHANISM OF ACTION.
Tafenoquine has been shown to have activity against both blood and liver stages of malaria even though the exact mechanism of action is not well established. It is believed that the active moiety of tafenoquine; 5,6 ortho quinone tafenoquine, seems to be redox cycled by P. falciparum which is upregulated in gametocytes and hypnozoites. Once inside, the oxidized metabolite produces hydrogen peroxide and hydroxyl radicals. It is thought that these radicals produce leads to the parasite death. Tafenoquine also inhibits heme polymerase just like the 4-aminoquinolones in blood stage of parasites which explains the activity against blood stages of parasites.
Studies have shown that tafenoquine is more potent (by a 10 fold) and less toxic than primaquine. The drug also has additional antiparasitic activity in mosquitoes, preventing sporozoite development in the mosquito.
In clinical trials, it was reported a tafenoquine-induced relapse prevention of 91.9% in cases of vivax malaria when pretreated with chloroquine. In prophylactic studies, tafenoquine showed an efficacy range from 84 to 87% against falciparum malaria and 99.1% against vivax malaria.source
STRUCTURE-ACTIVITY RELATIONSHIP (SAR)
From the structure:
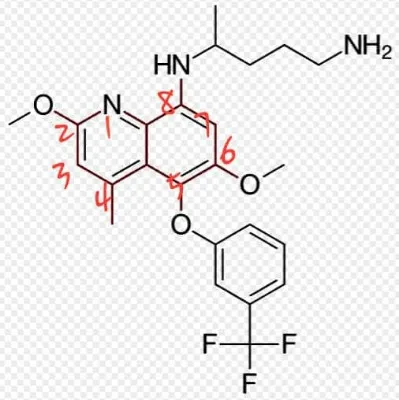
- The quinoline ring (the ring is coloured not so red) is responsible for the antimalarial activity.
- The classification of the compound is based on the amino group at position 8 of the quinoline ring
- OCH3 group at position 6 is not necessary for antimalarial activity, but when replaced by OC2H5, becomes less active and more toxic. When substituted by CH3, the compound becomes inactive.
- The substituted phenoxyl group at position 5 is inert to metabolism and protects the position 5 of the quinoline core from Phase 1 oxidation.
PHARMACOKINETICS
Tafenoquine is rapidly absorbed which is especially increased when taken with food. This helps to reduce adverse effects that concern the gastrointestinal tract. It is widely distributed in the body and has a long elimination half-life (approximately 16 days). This implies that the dosing interval for prophylaxis would be longer (than the usual once daily for 14 days of primaquine). Unlike primaquine, tafenoquine accumulates in the red blood cells, which may contribute to its greater potency compared with primaquine.source
TOXICITY .
The most frequently noted adverse events are mild stomach upsets, headaches, and muscular pains. As with primaquine, a major cause for concern is that of hemolytic anaemia in persons with a deficiency of the enzyme glucose-6-phosphate dehydrogenase (G6PD). More importantly, tafenoquine's slow elimination would result in sustained toxicity. Therefore, G6PD testing should be performed before administering the drug.source
CONCLUSION
In what would look like “turning around the tables” of this war, in favour of humans, it would seem that the theme for this year’s World Malaria Day: READY TO BEAT MALARIA, would be befitting. Earlier, the global response to malaria was regarded as being at a crossroads because the eminent victory we once envisioned somewhat became stalled. The FDA approval of Krintafel® can be regarded as a knockout punch for malaria, and to add more icing on the cake, a deathblow would be hopefully be delivered this year in the form of a malaria vaccine!
Approved by European regulators in July 2015, the vaccine, Mosquirix® (RTS,S), would be rolled out in selected areas of Ghana, Kenya and Malawi. The vaccine is the only licenced vaccine, to date, to show partial protection against malaria in children in large-scale clinical trials.source
Defeating malaria is absolutely critical to ending poverty, improving the health of millions, and enabling future generations to reach their full potential.
Tedros Adhanom.
What more could be more fulfilling than getting a nice spot to smile at the sun, rising over a large expanse of green vegetation, with the infinity gauntlet in your hand, knowing that you've disintegrated half of all female Anopheles mosquitoes in the universe! 😈
Thanks for reading.
P.S:
- Radical cure: is the use of a medicine that targets the dormant liver forms of the parasite, co-administered with currently available antimalarials such as chloroquine or artemisinin-based combination therapies (ACTs).
- Relapse: is when symptoms reappear after the parasites have been eliminated from blood but persist as dormant hypnozoites in liver cells.
- Recrudescence: is when the symptoms return after a symptom-free period. It is caused by parasites surviving in the blood as a result of inadequate or ineffective treatment.
REFERENCES
Centers for Disease Control and Prevention
Mechanism of Action of Tafenoquine
Pharmacokinetics of Tafenoquine
Structure-Activity Relationship
FURTHER READING
Mechanism of Parasite Resistance
Pharmacokinetics of Artemisinins
Why Tafenoquine has a Long Elimination Half-Life
Do you write #Science, #Technology, #Engineering and #Mathematics (STEM) posts? You can use the #steemstem tag. You can also join and become an active member of this great community on the DISCORD Server Channel.
If you are a Nigerian, and you write STEM-related posts, you can use the #stemng tag also.
