In order to get high levels of long-lasting antibodies, you need a good CD4+ T-cell response. These are also called helper T-cells and are the cells that are killed by HIV. When their levels dip too low, the whole immune system collapses, because their help is needed for so many immune functions. SARS CoV-2 also infects and kills CD4+ T-cells, although not nearly as much as does HIV.
T-cells, like antibodies, specifically recognize particular things. But while antibodies can recognize a wide variety of things, T-cells can only recognize small bits of proteins, and they can only recognize them when they are presented to the T-cells by MHC proteins. MHCs are like little molecular hands that hold out a small strand taken from a larger protein that was chopped to bits. The T-cells "feel" the hand with the bit of protein in it and can then activate.
Human MHCs are called HLAs. There is a lot of diversity of HLA genes in humans. Because they are so diverse, they are one of the main reasons that we need immunosuppression after organ transplantation, and why we try to match donor organs to recipients with as many HLAs in common as possible. You inherit your HLAs from your parents, and with them you inherit the ability to present a wide variety of protein bits. But it's not infinite, and for any given pathogen, there are some people in the population who are just better at presenting its protein bits to their CD4+ T-cells. If you a pathogen with a lot of different proteins, it can help to give your HLAs more options to find something that they can hold on to, but for SARS CoV-2, we would really prefer to make antibodies to spike, because that's the thing that binds to your cells.
The spike protein contains five protein sequences that can be presented by human HLAs. But for each of those five, some HLAs are better than others at holding it and presenting it to your T-cells. Some people have a mix of HLAs that are just better at presenting the bits of protein from the whole spike protein. That gives them more CD4 (and CD8) T-cells, which means that they get more antibodies, and probably longer lasting antibodies.
So just because some people have lower levels of antibodies doesn't mean that their immune systems are generally weak. They might be able to respond really well to something else. If you look at the data from Moderna showing response to boosters, there was a general trend for people who were low relative to everyone else before the booster to still be low relative to everyone else after the booster. But everyone's antibodies did still increase dramatically, to levels that are probably more than enough for awhile. So try not to stress if your levels are a bit below average.
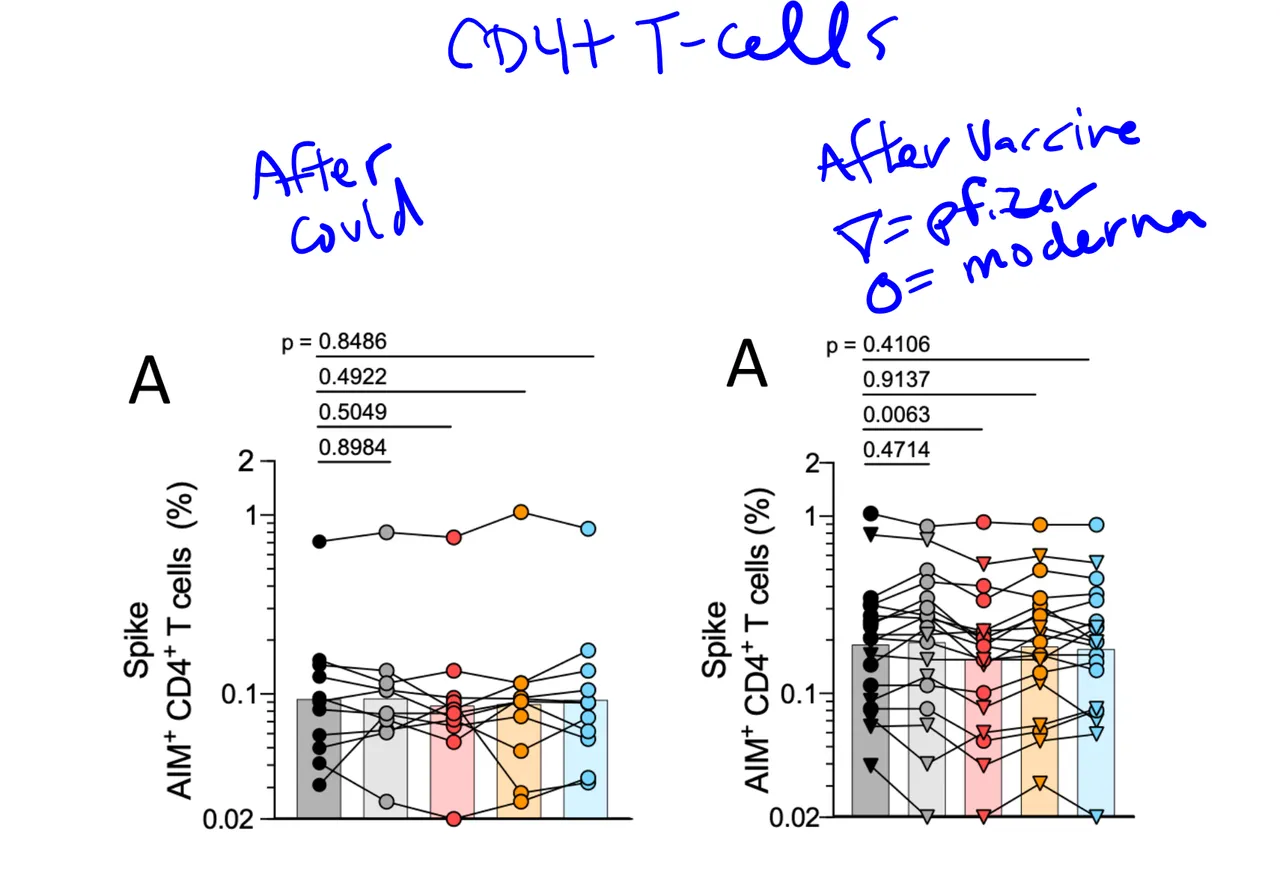
Also, if you look at CD4+ T-cells after vaccination vs after infection, the RNA vaccines clearly activate a lot more T-cells than does infection, at least on average. This is probably at least part of the reason that immunity from natural infection doesn't very long.
It's also clear that some people make a much better CD4+ T-cell response than others. There are some on the vaccine side that are pretty low, and one outlier on the covid side that is higher than a lot of the vaccine people. Measuring CD4+ T-cells is not easy, so I doubt there will be a commercial test any time soon, but your antibody levels, especially after 6 months or so, can give you a general idea